MANAGEMENT OF PATIENT WITH MAJOR BURNS
- It is important to remember a burned patient is also a trauma patient with the potential for other injuries beyond those related to the burn.
- Morbidity and mortality increases with increased BSA % of burn, in the very young or very old, and when pre-existing diseases are present such as cardiovascular, renal or pulmonary disorders.
- Standard approach to trauma is followed including assessment for C-spine and head injuries, pulmonary and abdominal trauma, fractures etc.
|
| Airway and Pulmonary Complications |
|
Carbon Monoxide Poisoning
- PaO2 may be elevated with a low oxygen saturation (carbon monoxide preferentially combines with hemoglobin instead of oxygen)
- pulse oximetry cannot distinguish between oxyhemoglobin and carboxyhemoglobin, resulting in falsely elevated SpO2 reading
- carbon monoxide toxicity contributes to the metabolic acidosis by limiting oxygen transport to tissues
- carbon monoxide levels must be directly meausred (not calculated) and are measured as carboxyhemoglobin on the CCTC GEM
- carbon monoxide binds to hemoglobin instead of oxygen as it has 280 times greater affinity for hemoglobin than oxygen. If the carboxyhemoglobin is 30%, the maximum oxygen saturation possible would be 70%
Upper Airway Obstruction Secondary to Edema
- superheated air typically causes injury to structures above the vocal cords; lower respiratory tract is not usually affected
- airway burns should be suspected if carboxyhemoglobin is high or burns occurred in an enclosed space
- edema with impaired upper airway patency may not occur for 12 to 18 hrs
- edema is progressive during the first 18 to 24 hrs - if airway burn is suspected, prophylactic intubation should be done early
- soot in the nares or mouth, or burned/swollen lips indicate that intubation is warranted
- a deep neck burn may cause external compression of the airway as the skin lacks the elasticity needed to accommodate tissue edema (compartment syndrome); escharotomy may be required
Chemical Burn to Upper and Lower Airways
- water soluble gases found in smoke from burning plastics or rubber reacts with water in mucous membranes to produce strong acids and alkalies
- may cause bronchospasm, ulceration, edema and damage to ciliary mechanism
- lipid soluble compounds are transported to lower airways on carbon particles and produce cell membrane damage and alveolar flooding
- pulmonary infections are common
- corticosteroids increase mortality and are contraindicated
- only treat infections documented on culture (to reduce chance of developing infections with resistant organisms)
- pulmonary edema may develop as a consequence of profound hyponatremia associated with burns, excessive fluid resuscitation or renal failure
Impaired Chest Wall Compliance
- present with full thickness burns to thorax due to loss of elasticity of skin
- full thickness burns to abdomen can impair ventilation due to abdominal compartment syndrome
- increased chest wall resistance from burned skin can lead to laboured breathing and rapid respiratory deterioration
- increased CVP secondary to raised intrathoracic pressures can accelerate the rate of protein and fluid loss into the burn tissue and increase the chest wall edema
- urgent escharotomy is required on admission, and should extend into fat and possibly through the fascia
Monitoring and Management
- maintain 100% oxygen therapy to enhance oxygen binding with hemoglobin until the carboxyhemoglobin is < 5% (0.05); 100% oxygen decreases the half life of carbon monoxide to 45 minutes and enables oxygen to "push" carbon monoxide off the hemoglobin by maintain a higher part pressure of oxygen)
- monitor carboxyhemoglobin and TRUE (not calculated) oxygen saturation available on the CCTC Gem or in the core lab
- pulse oximetry is unreliable - it overestimates oxygen saturation if carbon monoxide or methemoglobin levels are increased because the pulse oximeter cannot differentiate between the two wavelengths; it would be safer not to measure pulse oximetry until the carboxhemoglobin normalizes (< 5% or 0.05)
- monitor for metabolic acidosis or lactic acidosis - can develop as a result of carbon monoxide poisoning or cardiovascular shock
- assess for evidence of inhalational injury (suspect if burn occurs in enclosed space, carboxyhemoglobin is elevated or soot is present
- soot, singed airways, stridor, hoarseness or wheeze indicates need for intubation - AIRWAY EDEMA WILL GET WORSE OVER INITIAL 24 HRS - PROPHYLACTIC INTUBATION IS INDICATED IF EVIDENCE OF AIRWAY BURNS ARE PRESENT ON ADMISSION!
- bronchoscopy may be performed to assess airway for injury
- be careful not to cut the endotracheal tube too short - leave several inches of endotracheal tube beyond the mouth to allow for facial and lip swelling (which can be extensive!)
- observe for neck burns that could further compromise airway; circumferential neck burns can cause compartment syndrome with compession of the cerebral circulation or airway
- monitor respiratory status for increased RR rate, effort, minute volume and blood gases - monitor closely for need to mechanically ventilate
- depolarizing agents such as succinylcholine are CONTRAINDICATED if neuromuscular blockade is required for intubation - use non-depolarizing agents such vecuronium if required (deplolarizing agents may worsen hyperkalemia)
- increased effort, peak airway pressures or CVP could indicate compartment syndrome secondary to thoracic or abdominal burns, hemo/pneumothorax or pulmonary edema
- difficulty with clearance of secretions increases risk for secretion retention; PEEP, Bronchodilators, frequent suctioning and chest physiotherapy important
- monitor for signs of pulmonary infection
- there is mixed evidence on the role of nebulilzed n-acetylcysteine alternating with inhaled heparin; this is primarily before after restrospective data
- our protocol has included heparin 5,000 units per dose, however, there is some evidence that doses of heparin 10,000 alternating with n-acetyl cysteine Q4H are needed to produce a benefit (so that the patient receives one drug every 2 hours); heparin at these doses may be associated with shorter time on the ventilator and a reduction in lung injury scores
- a randomized placebo control trial is currently underway
- although there is no evidence for benefit or harm, regular inhaled bronchodilators are routinely ordered in many burn centres
- the routine use of inhaled steroids without other indications is not recommended
|
| Cardiovascular Complications |
|
Burn Shock
- the result of massive fluid shifts where intravascular volume is lost into burned and nonburned tissue
- increased vascular permeability, raised tissue osmotic forces and cellular swelling contribute to the loss of intravascular volume
- myocardial depressant factor may contribute to shock by decreasing myocardial contractility
Burn Edema
- during the first 6 to 8 hours, there is a large loss of protein rich fluid from the intravascular compartment to the interstitial fluid, due to vascular permeability
- intravascular protein loss results in a loss of the protein gradient between the plasma and interstitium
- interstitial edema fluid forms a gel after approximately 12 hrs and leads to obstruction of local lymphatics
- tissue oxygen tension decreases with edema as distance for oxygen delivery increases
- the increased permeability gradually returns to normal by 24 hrs
Changes in Nonburned Tissue
- fall in intravascular colloid pressure drives fluid into interstitium
- vascular permeability is only minimally affected
- impairment of Na/K ATPase leads to a shift of sodium and water from the extracellular space into the cell
- ATPase is normalized by 24 hrs if fluid resuscitation is adequate
Hypermetabolic State
- beginning at day 5, there is a gradual increase in the metabolic rate to levels ranging from 2 to 2.5 X normal at day 10
- characterized by increased oxygen consumption (cardiac output and minute volume), heat production, body temperature, hyperglycemia and protein catabolism
- cardiac output and CO2 production can double
- augmented enteral feedings should be initiated within 48 hrs of the burn injuries
- inflammatory mediators generate SIRS (systemic inflammatory response syndrome), increasing the potential for circulatory failure
Monitoring and Management
Pharmacological Support
- inadequate volume resuscitation should be considered as the main cause for hypotension in the first 3 days, and following debridement of wounds
- inotropes may be required if hypotension persists despite fluid replacement
- beyond 3 days, increasing need for inotropes or vasoconstrictors may indicate development of septic shock
- monitor for signs of infection or sepsis; rarely, sepsis may occur early secondary to very deep or contaminated burns
Fluid Management
- monitor BP, HR and urine output closely (as evidence of adequate fluid resuscitation)
- monitor electrolytes, especially potassium and sodium
- fluid resuscitation is the cardiovascular priority in burn management
- the larger the area of burn, the more significant the fluid deficit
- the goal is to achieve a balance between the restoration of adequate tissue perfusion while minimizing edema formation
- administer Lactated Ringers as initial fluid resuscitation.
- Parkland Formula
The Parkland Forumula was one of the most commonly used strategies for burn fluid resuscitation. The original formula included ringers lactate at a dose of 4 ml per kg per % body surface area. A total of 50% of this dose is given in the first 8 hours with the remaining 50% given over the next 16 hours. At 8-10 hours, the infusion should be lowered to the lowest amount possible to maintain hemodynamic stability.
Avoid very rapid bolus administration at the onset of resuscitation as this likely forces large volumes of fluid out of the vessels and into the inflammed tissues to make tissues more edematous.
At 8-24 hours, an infusion of 5% Albumin may be introduced at 8 to 24 hrs as a drip at the rate of 0.5 mL to 1.0 mL/kg/% BSA burn.
- MODIFIED PARKLAND FORMULA and current controversies
Similar to the evolution of sepsis resuscitation, there is increasing concern that excessive fluid resuscitation is harmful. Over resuscitation can lead to edema, compartment syndrome and burn edema. Burn edema can adversely effect burn care and grafting. Conversely, dehydration can also adversely affeect burn grafts. There is limited evidence regarding the most appropriate resuscitation strategies.
A more conservative approach to fluid resuscitation is being advocated. This can be achieved by using a modified Parkland Formula:
- Calculate 24 hour fluid requirements as 2 - 4 ml per kg per % body surface area.
- Administer 50% of this volume over the first 8 hours and remaining volume over the next 16 hours. Calculate from the time of injury, not the time of admission.
- Target fluid resuscitation to the end point of a urinary output of 0.5 - 1 ml/kg/hour (adults) and 1 - 1.5 mL/kg/hour (children). Avoid over-resuscitation
- Consider 5% albumin at 0.5 to 1.0 mL/kg/% BSA burn after 8 to 24 hours. Some formulas use 25% albumin.
Albumin has been part of fluid resuscitation in burn care since the 1940's. While recent controversy has emerged regarding its safety, a 2018 Cochrane Systematic Review did not find any mortality difference.
- Vasopressors may be considered if necessary to maintain perfusion pressures. If vasopressors or required, sepsis should be ruled out.
- Caution: Burned patients who have also experienced trauma may have higher volume and blood product requirements. Burn injuries may mask other injuries.
- Blood products may be required after burn debridements.
|
| Renal Complications |
|
Secondary to Burn Shock
- renal blood flow should be monitored closely to reflect the adequacy of systemic perfusion during the early phase of injury; the target urine output is 0.5 to 1.0 mL/kg/h
Secondary to Rhabdomyolysis
- compartment syndrome can develop as a result of loss of tissue elasticity
- compartment syndrome requires early escharotomy to preserve tissue perfusion (late escharotomy can result in the release of lactic acid, potassium and other metabolites from dead tissue, with subsequent cardiovascular collapse)
- rhabdomyolysis (or breakdown of skeletal muscle) can occur as a result of compartment syndrome or burn injury
- rhabdomyolysis is diagnosed by elevated serum myoglobin and myoglobinuria
- to prevent renal failure if rhabdomyolysis occurs, increased fluid resuscitation, aggressive diuresis and alkalinization of the urine with a bicarbonate infusion is required
- monitor urine myoglobin and treat rhabdomyolysis
- monitor for compartment syndrome and treat early with escharotomies
- hyponatremia is common due to loss of sodium through the burn wound and dilution during fluid administration
- hypokalemia is common during resuscitation and can be exaggerated by nasal gastric loss or diarrhea
- kayexalate or insulin/dextrose to treat early hyperkalemia is not recommended; hyperkalemia will usually resolve with fluid resuscitation and correction of acidosis
- hyperkalemia can develop early in the burn injury as a result of metabolic acidosis and the release of potassium from damaged cells
- monitor urine output, creatinine and urea
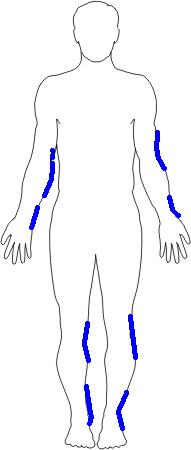
| Preferred Sites for Escharotomy |
|
Monitoring and Management
|
| Thermoregulation |
- with a deep burn, the barrier to evaporative water loss is impaired, promoting heat loss
- heat loss can lead to an increased metabolic rate as the burn victim attempts to maintain body temperature
- heat loss is decreased by covering the wounds and maintaining high room temperatures
|
| Wound Care |
Cleansing
- keep wounds covered to minimize infection
- avoid prophylactic systemic antibiotics - not useful because wounds are avascular and antibiotics may promote the growth of resistant organisms
- topical antibiotic creams such as Flamazine control bacterial counts and increase comfort
- aggressive wound debridement is essential to the removal of potential sources for infection such as bacteria and necrotic tissue
- eschar (dead tissue) must be removed with scissors and forceps or scalpels; small areas can be debrided during routine burn dressing changes
- wet to dry dressings and scrubbing of wounds during dressing changes can enhance mechanical debridement
- enzymatic debriding agents may be ordered to loosen eschar and promote removal, particularly in patients unable to go to the OR
- frequent surgical debridement is optimal to remove non-viable tissue; bleeding and fluid loss is generally significant after debridements
- monitor all wounds for purulent drainage or signs of infection
Grafts and Dressings
- polyurethane film is useful for simple partial thickness burns or donor sites
- hydrocolloid dressings may be used on donor sites, but they limit the ability to observe the site and are not recommended for burned sites
- deep partial thickness and very small full thickness burns will heal spontaneously; should be dressed with bacitracin and adaptic dressing
- autografts (from an uninjured area of the patient's own skin or from an identical twin) provide the only permanent graft material; grafting shortens healing time and improves the cosmetic appearance of deep partial burns, and is mandatory for the healing of full thickness burns (decision to graft may be based on the total % BSA burn and the need to conserve donor sites for full thickness injuries
- in large area burns, the same graft donor site may need to be used repeatedly as the only source for graft material; protection of this donor site from infection is critical
- when autograft sites are sparse, donor skin can be minced and placed into a growth medium to increase the number of epithelial cells or small pieces of donor skin can be dropped across a large burn (in an attempt to increase the benefit from a small donor area)
- cadaver skin (allograft or homograft) can be used as a temporary dressings - allografts will promote vascular ingrowth to seal the wound against bacterial invasion, however, they will be rejected within about 2 weeks
- xenografts/heterographs (from other species) such as porcine grafts can also provide temporary wound dressings - place pigskin dermal side onto the wound (the dermal side faces the centre of the roll - the graft will roll towards the dermal side)
- porcine grafts should be removed in 3 - 4 days or if purulent discharge is noted (porcine grafts may be digested by the wound, becoming a source for bacterial growth)
- scarlet red or xeroform dressings are used to protect the donor site; as the site heals, the edges of the dressing dry and curl - trim the loosened edges gradually until the entire wound heals (do not forcefully remove donor dressings or wound healing will be disrupted)
- tubular support dressings provide pressure in the range of 10 - 20 mmHg and are applied 5 - 7 days after grafting to minimize contracture formation
Dressing Routines
- pain management is a priority
- coordinate physiotherapy with dressing changes
- splint limbs to minimize contractures and maintain functional position of joints
|
| GI Function |
|
Monitoring and Management
- gastric dilation and ileus is common in burns > 20% BSA
- GI function should return in 24 - 48 hours
- increased stress hormone output increases the risk for Curling's ulcer
- gastric drainage on admission minimizes gastric distention, emesis and risk for aspiration
- feeding should be initiated as soon as possible; burned patients have high caloric requirements due to wound healing and the increased catabolic state
- careful nutritional assessment is needed to ensure adequate caloric intake
- metabolic rate calculations with the metabolic cart can assist in providing appropriate nutritional support while monitoring for excessive carbohydrate loading (which increases demands on the cardiorespiratory system)
- GI prophylaxis with H2 blockade is important due to high risk for stress ulceration
- monitor for return of bowel function
- monitor for evidence of GI bleeding, anemia or occult rectal blood
Determination of Burn Type
Calculation of Percentage of Burns
|
Derek Brzozowski and Brenda Morgan. (October 23, 2000)
Updated: January 14, 2019
References:
Buck, D., Fedorowicz, Z., and Ehrlich, A. (2018). Major burns. DynaMed updated October 23, 2018.
http://web.a.ebscohost.com.proxy1.lib.uwo.ca/dynamed/detail?vid=2&sid=af18d660-cd94-4141-84d3-54691187c6f0%40sessionmgr4007&bdata=JnNpdGU9ZHluYW1lZC1saXZlJnNjb3BlPXNpdGU%3d#AN=113804&db=dme
Deutsch, C., Tan, A., and Smailes, S., and Dziewulski, P. (2018). The diagnosis and management of inhalation injury. Evidence based approach. Burns, 44, 1040-1051.
Endorf, F and Dries, D. (2011). Burn resuscitation. Scandinavian Journal of Trauma, Resuscitation and Emergency Medicine. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3226577/pdf/1757-7241-19-69.pdf
Lewis, et al. (2018). Colloids versus crystalloids for fluid resuscitation in critically ill people. The Cochrane Collaborative. Wiley and sons.
Prasad, P., Lang, E., and Trow, T. (2015). Toxic inhlational injury. Updated March 5, 2015. http://web.a.ebscohost.com.proxy1.lib.uwo.ca/dynamed/detail?vid=4&sid=af18d660-cd94-4141-84d3-54691187c6f0%40sessionmgr4007&bdata=JnNpdGU9ZHluYW1lZC1saXZlJnNjb3BlPXNpdGU%3d#AN=906193&db=dme
Soussi, S., et al. (2018). Early hemodynamic management of critically ill burn patients. Anesthesiology, 129 (3), 583-595.
-