Overview of Safety Protocol: Prevention of Iatrogenic Pneumothoraces The procedure for the insertion of any feeding tube in CCTC (gastric or small bowel) requires a TWO step process. Try to coordinate Step One to other routine Xray's if the timing is appropriate to reduce the number of Xrays. The goal of Step One is to rule out airway placement and confirm esophageal insertion before advancing additional feeding tube into the patient. Step One confirmation is completed by CHEST Xray. The feeding tube tip must be below the level of the carina and there must be confirmation that the feeding tube has not followed either the right or left main stem bronchus.
Optimally, the tip of the feeding tube should be inserted no greater than 5 cm below the carina (to reduce the risk for distal airway advancement and potential pneumothorax). Step One must be confirmed before the tube can be advanced to the stomach or small bowel. Examine the feeding tube distance marking following completion of the Step One Xray. If the feeding tube tip distance is optimal on chest Xray, document the insertion distance on the Kardex to inform future insertions (e.g., from the right nare optimal Step One distance is 35 cm). If the Step One chest Xray demonstrates that the feeding tube tip was greater than or less than optimal, modify the recommended distance before documenting to the Kardex.
Step Two confirmation is completed by ABDOMINAL Xray following advancement of the feeding tube to the stomach or small bowel. This must be completed before a patient can be fed. Optimizing Small Bowel Placement:
To reduce the chance of coiling of the feeding tube within the stomach and to optimize tube placement within the small bowel (ideally to the jejunum), limit the amount of tubing that is initially advanced during Step Two to 80-90 cm. After the abdmonial Xray is taken, leave the patient on the Xray plate while the Xray is examined. If the feeding tube tip has successfully entered the duodenum, advance the remaining tube (or until resistance is met) with the patient still on the Xray plate. Repeat the abdmoinal Xray after advancement and ensure that the final image is uploaded to Power Chart as placement confirmation. If the feeding tube is coiled in the stomach at 80-90 cm, do not advance the tube any further. Remove the wire and attempt gastric feeding (advancing more tube leads to large loops of coiled feeding tube). Goal for Step One Placement:
|
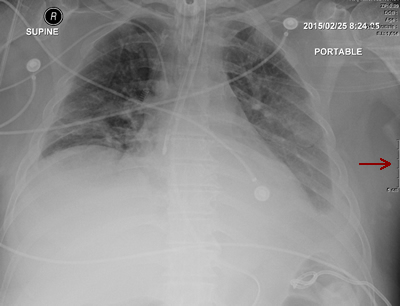
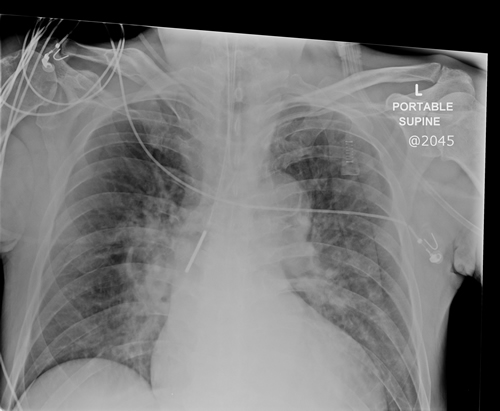
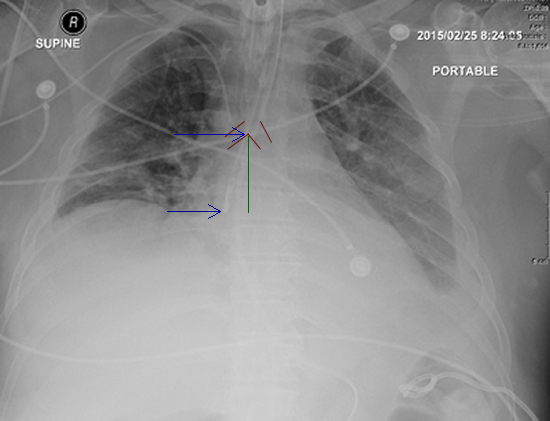
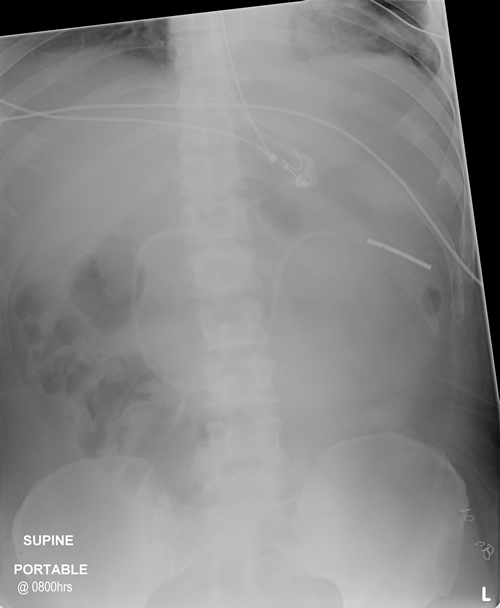
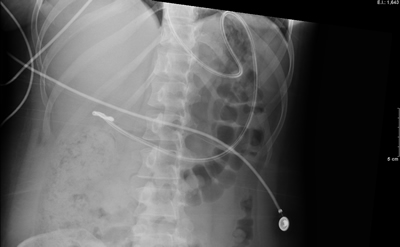
| | Image 1: Chest Xray successfully rules out airway placement. You can use the ruler (red arrow) to measure the distance of the tip from the carina. Step back to view the darkened area of the trachea and branching of the left and right bronchi. The tip of the feeding tube must be below the level of the carina and it should not follow either airway. If the tube is more than 5 cm below the carina, it has been advanced more than needed to rule out airway placement. | Image 2: This tube is in the right mainstem bronchus. The proximal location has successfully identified airway placement, without the harm associated with a more distal advancement. The tip is less than 5 cm beyond the level of the carina which is optimal. Reattempt insertion after removing the feeding tube completely. Use this same distance for the next attempt. | | | Image 1b: The carina is identified by the top blue arrow. The green line shows the distance from carina to feeding tube tip. |
| | Image 3: To determine the distance from the tip of the carina, you can click on the ruler from the Centricity menu bar. Drag the line between the carina and the tip of the feeding tube. In Power Chart the line length will be displayed as 50 mm (maximum distance from carina = 5 cm). In PAX display you can use the cm markers identified by the red arrow in Image 1. |
How to estimate the optimal length for Step One: 1. Look at the Kardex to see if the optimal distance has been recorded from a previous attempt 2. Measure from the tip of the nose to ear to xyphoid process and SUBSTRACT 10 cm from the measured length. 3. Oral route: look at the distance marking for the endotracheal tube and ADD 5 cm. 4. Nasal route: look at the distance marking for the oral endotracheal tube and ADD 10 cm. Following the initial Xray, look at the distance marking for the feeding tube and compare it to the Chest Xray. There can be a lack of precision in the estimation of the optimal insertion distance, especially on the first attempt. If the first Chest Xray reveals that the tube was advanced further (or not far enough) than needed to rule out lung placement, use the Chest Xray and ruler (shown above in Image 3) to identify the optimal insertion distance for future attempts. Use this information to recommend the distance for future insertions by adjusting the insertion distance. Record the recommended distance for Step One on the Kardex to inform future insertions. When documented the optimal insertion distance on the Kardex, be sure to identify whether this was an oral or nasal insertion. Two Examples of Step One Insertion depth that is greater than the Goal: |
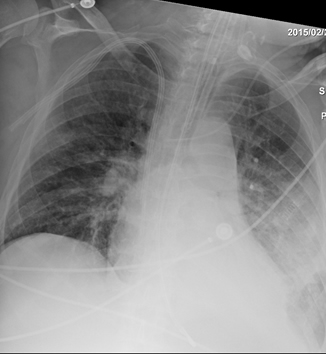
| | Image 4: Although this Step One Xray rules out airway placement, this tube was advanced further than desired. The tip was in the stomach. If this tube had entered the airway, lung trauma would have been likely. Document the modified insertion distance on the Kardex to inform future insertions. | Image 5: Although the Step One Xray successfully identified right airway placement prior to further advancement, this tube was advanced too far (with greater risk for harm). Document the modified insertion distance on the Kardex to inform future insertions. |
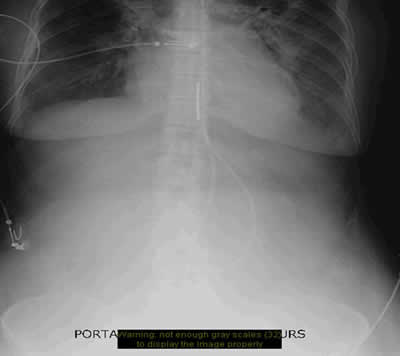
Step Two includes the advancement of the feeding tube, aided by the prior administration of a prokinetic, right sided positioning and administration of air (do not perform any steps that are contraindicated, just perform the ones that are acceptable in this patient). An abdominal Xray is required following the final advancement, even if the tube was intially observed in the stomach. Feeding tubes can coil and loop back on themselves and end up with the tip in the esophagus. The only way to ensure that the tube has not kinked backward is via the Abdominal Xray. Example of Optimal Small Bowel Placement: | | Image 6 (above): The feeding tube tip enters the duodenum toward the right. Note that the tube takes a downward turn if it enters the duodenum. The tube continues through the ~ 10 cm of duodenum and turns downward to the left of the sternum as the tube likely enters the jejunum. |
Other Examples:
|
| | Image 7 (above): This feeding tube appears to have entered the duodenum but the tip looks to be kinked. Continued advancement of large amounts of tubing can lead to problems seen in Image 10 | Image 8 (above): This feeding tube appears to have "turned the corner" into a downward direction that would suggest it is in the very beginning of the duodenum. The hard part is done! Advancing the tube further before removal of the guidewire will usually result in the optimal placement seen in Image 6. |
|
| Image 9 (above): This Xray reveals the reason why an Xray should be performed after a tube is advanced. This tube has curled back from the stomach and is heading back up the esophagus instead of toward the duodenum. Feeding here would lead to aspiration. This tube should be pulled all the way back out. Attempts to pull back a few cm will only result in less loop; the tip direction will remain backwards. Tubes can kink/fold within the bowel and take a backward journey as well. | Image 10 (above): The tip of this tube is curling upward from the point where the duodenum is expected...this is curling in the stomach (a tube that enters the duodenum heads downward). Because the tube did not enter the duodenum and a significant length was added, there is a lot of surplus feeding tube in place. Several cm of tubing should be withdrawn before the guidewire is removed. Leaving the loop of tubing can lead to knotting. |
PROCEDURE FOR INSERTION OF GASTRIC AND SMALL BOWEL FEEING TUBES |