Set the Drainage Level - Obtain an order for the level of the drainage chamber.
- Orders should include a maximum CSF volume to drain and both a MINIMUM and maximum lumbar ICP. The minimum is used to prevent ventricular dehydration which may increase for bleeding.
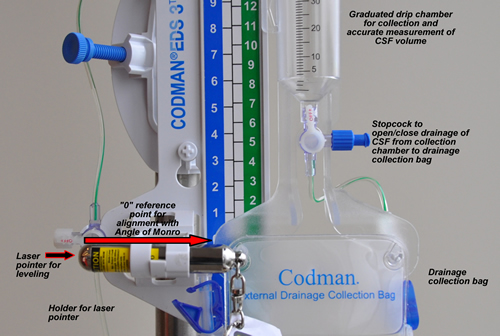
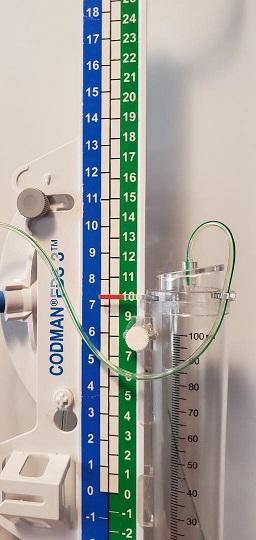
- Loosen the buretrol adjustment screw and move the drip chamber until the small arrow is aligned with the desired height.
- Tighten the screw to secure the buretrol position.
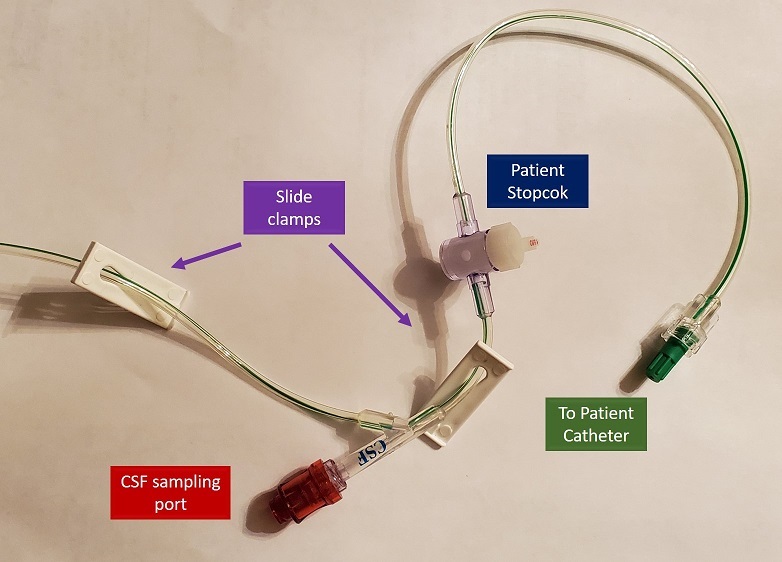
If the "0" reference is level with the patient's catheter, a drainage level of 10 cmH20 above the lumbar space provides automatic "venting" of CSF if the pressure rises above 10 cmH20. If the "0" reference and the drip chamber are both positioned level with the catheter, drainage would occur the moment the lumbar CSF pressure > 0. Normal lumbar CSF pressure is < 10 mmHg. This could lead to over drainage and potential for cerebral bleeding. Weaning of the drainage system can be done by raising the level of the drainage unit (the ICP would have to be higher before drainage would occur). Intermittent drainage may also be initiated, where pressure is monitored and drainage only opened if the pressure exceeds a specific level. Both the patient and mounting panel stopcocks must be open between the patient's catheter and the drainage chamber for drainage to occur. When the system is left continuously open to drain and the drainage chamber is positioned to initiate drainage at a set level, pressure is maintained at a more consistent level. Note that the bedside monitor measures pressure in mmHg; 10 cmH20 is the same as 7.4 mmHg. Thus, a properly positioned unit with the drip chamber at 10 cmH20 will drain if: - the stopcocks are open between the patient's catheter and the drip chamber
- the pressure in the lumbar space exceeds 10 cmH20 (or exceeds 7.4 mmHg on the bedside monitor).
- the catheter/circuit is patent (e.g. free of clot or debris)
- there is fluid in the lumbar space (if the pressure is high due to cord edema, there may not be any CSF to drain)
If the circuit fails to drain despite a pressure on the monitor that is > than the level of the drainage chamber, patency can be assessed by lowering the entire drainage unit to below the head. Notify CCTC resident AND Vascular Surgery if the unit fails to drain in the presence of an elevated pressure despite troubleshooting efforts A typical order is "10 cmH20" above the lumbar space. The right hand (green) column of numbers of the Codman drainage unit is in cmH20. The column to the left (blue) displays the equivalent pressure in mmHg (7.4 mmHg - 10 cmH20).). In the example of "10 cmH20", the system is correctly placed if the "0" reference point is level with the patient's iliac crest and the small arrow is aligned at the 10 cmH20 marking, drainage would be expected if the bedside monitor identifies a pressure > 8 mmHg. If the lumbar drain is in the open position, raising the head of bed can increases the pressure gradient between head and lumbar spine and can lead to over-drainage. Continuous drainage is safest with the HOB close to flat. Excessive fluid removal or reduction in the intracranial pressure can increase the risk for intracranial bleeding. Turn stopcock off temporarily any time the drain needs to be moved to below the reference level. A minimum ICP should be identified to prevent intracranial dehydration which may increase risk for bleeding. Turn drain off to drainage if output exceeds ordered maximum (usually 10-20 ml/hr). If pressure is low, an order to raise the drain level or to switch to intermittent drainage may be indicated. |