ANTIMICROBIALS; ANTIBIOTICS; ANTIFUNGALS; ANTIVIRALS; CULTURES
Antimicrobials describe a broad group of drugs that are used to kill pathogens (germs that are foreign and potentially harmful to an individual) or impair their ability to reproduce. Within this category are several subgroups of antimicrobials.
Antibiotics are drugs that have a specific action against bacteria. These are the most commonly used antimicrobial agents. Antibiotics do not work against viruses and should not be used to treat viral infections. Penicillin was the first antibiotic ever developed. We now have many organisms that are resistant to penicillin drugs (penicillin no longer works).
Antifungal agents are drugs that specifically attack fungal or yeast infections.
Antiviral agents are drugs that work to interfere with the ability of a virus to replicate itself (make copies of itself). The effectiveness of antivirals depend upon the type of virus. Antivirals are not effective for all viruses, and most infections due to a virus will resolve without treatment. An example of a virus is influenza. Tamiflu is an example of an antiviral agent that may shorten the duration of some forms of Influenza.
Although antibiotics are not effective against most viral infections, patients may develop bacterial infections while being ill with a virus or after recovering from a viral infection (e.g. they may develop a bacterial pneumonia). This bacterial complication may be treated with antibiotics.
Antimicrobial Stewardship: The CCTC participates in an antimicrobial stewardship program that includes a Critical Care Consultant, an Infectious Disease physician (a physician who specializes in infections and antimicrobial therapy), an Infectious Disease Pharmacist and a CCTC Pharmacist. This team reviews the cultures and antimicrobial therapies for of all patients in CCTC. This program helps to reduce inappropriate antimicrobial usage and ensures the best agent is used when treatment is needed.
CULTURES
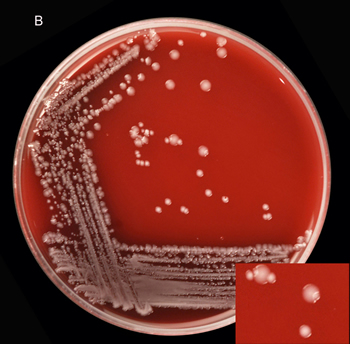
Antibiotics are not all equal. Antibiotics that are effective against one type of bacteria may not work against another. To select the best antibiotic, samples of infected drainage or fluid are collected from the patient and sent to the lab for "culture". A sample of the fluid is rubbed over a special culture plate (Image 1). This plate provides an environment that encourages the pathogen to grow. After a day or more, the culture is examined under a microscope to identify the shape and characteristics of any bacteria. This allows the physician to choose antibiotics that will work against a particular category of bacteria. The final report provides the specific type and strain of the microorganism. The lab will not describe a culture as "negative" (no growth of pathogens) until the culture has been monitored for several days. This is why it can take several days for a culture report to come back.
Image 1: Bacteria growing on a culture plate
Once the bacteria has been defined, the lab technologist performs other tests to identify the antibiotics that are capable of killing the organism. This is called sensitivity testing. If a patient appears to be unwell, we will usually start "broad spectrum antibiotics" (antibiotics that will cover a wide range of bacteria) until all of the test results are completed. Once the sensitivity testing is available, we may change the antibiotics to one that is more specific. If the bacteria is resistant to the antibiotic that was chosen, it will need to be switched ton one that works agains the organism that is making the patient ill.
Antibiotics that have the "broadest" action are called Broad Spectrum Antibiotics. Broad spectrum antibiotics are very valuable when we do not know the cause of the infection, especially when patients are very ill. Unfortunately, they may also be more toxic to some of the body's organs (e.g., the kidney) and are more expensive. They may also kill our "good bacteria", allowing other bacteria to take over. As soon as we know the actual cause of the infection, the antibiotics are "fine tuned" by changing the antibiotic to one that is more bacteria specific. We are careful to avoid over-use of antibiotics due to the risk that bacteria might become resistant to our antibiotics.
When patients are admitted with a serious infection, one of the hospital Infectious Disease Physicians may be consulted to work with our CCTC physicians to select the best treatment. This is in addition to our Antimicrobial Stewardship Program.