|
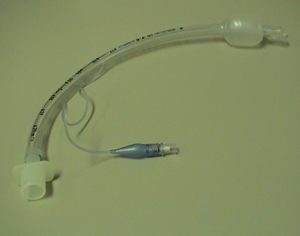
ENDOTRACHEAL TUBE; ETT "Endotracheal" means "through the trachea". It is a term that describes a breathing tube that is inserted through the windpipe or trachea. It is commonly called an ETT or ET tube. An endotracheal tube is an example of an artificial airway. A tracheostomy is another type of artificial airway. The word intubation means to "insert a tube". Usually, the word intubation is used in reference to the insertion of an endotracheal tube (Image 1). Patients may need an endotracheal tube for one of several reasons. An endotracheal tube is needed to mechanically ventilate a patient (or breathe for them by a machine). Each breath is pushed into the endotracheal tube and into the lung. An endotracheal tube is also needed if a patient is unconscious or has a brain injury. The brain controls the reflex in the airway that prevents choking when we swallow or eat. This reflex is called the gag reflex. The top of the windpipe has a special opening called the epiglottis. When we swallow food, the epiglottis closes to prevent food from entering the windpipe. When patients are heavily sedated, unconscious or have a brain injury, this protective response is often impaired. Without a gag reflex, saliva would enter the windpipe. This is called aspiration. Aspiration is a serious complication and one of the causes for pneumonia. A less common reason for intubating a patient is to keep the airway open. This is seen most commonly in patients with tumours or growths in the neck or upper chest. The usual route for inserting an endotracheal tube is through the mouth. This is called an oral endotracheal tube. Less frequently, the endotracheal tube is inserted through the nose. This is called a nasal endotracheal tube. A soft donut shaped balloon is located around the outside of the endotracheal tube. This is called the "cuff" (Image 2) . The cuff is inflated with air, and serves two purposes. First, it reduces the number of oral sections that can travel down the outside of the tube and into the lung. This is important because inserting an endotracheal tube into the airway will "wedge" the epiglottis into an open position. Although the cuff reduces the amount of secretions that can enter the lung, it does not completely prevent it. For this reason, patients on ventilators are at risk for developing pneumonia from secretions. The second reason for the cuff is to keep any mechanical breaths from leaking out of the lung around the tube. When we give a patient a breath with the ventilator, we want the breath to go in and out through the tube. Without a cuff, the breath would go in the tube but part of it would escape around the cuff before it was able to reach the lung. As long as the patient has an endotracheal tube in place, the cuff will need to be inflated. An inflated cuff will prevent the patient from being able to speak. Speech is produced when we exhale air through the vocal cords, causing them to vibrate. Because the cuff blocks the flow of air around the tube, speech is not possible. Once the tube is removed (called extubation), the patient will be able to speak. The voice may sound hoarse and the patient may have some throat discomfort for the first few days. Preventing Ventilator Associated Pneumonia (VAP) or Aspiration (choking on secretions) Pneumonia is a serious complication of mechanical ventilation and breathing tubes. We participate in the Safer Healthcare Now! VAP reduction campaign. Because the cuff on the breathing tube only reduces (doesn't prevent) secretions from getting past the cuff, we have a number of other strategies that are part of routine practice:
|
Image 1: Patient with an oral endotracheal tube. |
|
|
Image 2: Endotracheal tube showing inflated cuff. |
||
|
|
||
|
||
Last Updated: October 23, 2014