November 8, 2022
Medical Imaging is considered the “eyes of medicine.” Medical Radiation Technologists (MRTs), and when referring to ultrasound, Diagnostic Medical Sonographers (DMSs), are the healthcare professionals who capture images of the body to aid in the diagnosis, monitoring and treatment of a variety of medical conditions. They use some of the most advanced technology in healthcare and each piece of technology results in a specific type of image. This technology has seen significant advances over the years and has helped transform medicine by changing the way diseases are identified and diagnosed. For Medical Radiation Technologist (MRT) Week (November 6 to 12), we spoke with seven MRTs about their particular medical imaging modality, how the technology they use uniquely captures images of the body and why they find their role so rewarding.
Karly Brown, MRT (R), Medical Radiation Technologist - Radiology
What are some unique aspects to your role in Radiology and how does it help with patient care?
As radiology technologists, we are responsible for providing diagnostic x-rays to all areas of the hospital. In the Radiology Clinic we see a great deal of orthopaedic outpatients for pre-operative and post-operative imaging. We are also responsible for providing any requested x-rays to our inpatients, including portable imaging, fluoroscopy imaging in the operating room, imaging for procedures such as modified barium swallows and mini-cat scans, 24/7 imaging in the emergency department, and specialized imaging for outpatients at the Fowler Kennedy Clinic.
A large amount of our imaging is performed to diagnose fractures, chest imaging for chest pathology diagnoses, and routine follow ups to aide in patient treatment plans. Our x-ray imaging services are a crucial tool in diagnosing our patients and will often provide a means to the next step of their treatment. The patients we see are usually experiencing some, if not a great deal, of pain, and we are here to provide them with as much comfort and kindness as possible.
Radiology is largely collaborative with many other areas of the hospital in providing patient care, therefore, we must provide adaptability, understanding and empathy when working together to care for our patients.
Is there any exciting news to share about recent technology upgrades at LHSC in your modality?
The UH Radiology department has recently onboarded several new x-ray machines. While it has been a learning curve, the technology is far more advanced than our previous equipment, which is of great benefit to our department productivity and overall patient care.
What do you find is the most rewarding aspect of your work?
I take pride in providing high quality diagnostic imaging to our patients and strive to provide them with the highest level of patient care. Aside from patient care, the most rewarding aspect of this career for myself is the team of technologists I am honored to work alongside every day.
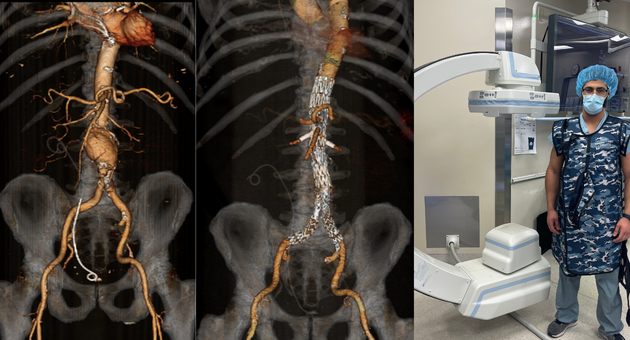
Frank Franze, MRT (R), Medical Radiation Technologist - Vascular Interventional Radiology (IR)
What are some unique aspects to your role in Vascular IR and how does it help with patient care?
There are only a few of us trained in the hospital to do our job, and we work side by side with the vascular surgeons and nurses to provide angiography. Angiography is an imaging technique which is used to visualize the inside of blood vessels, particularly the arteries. The specialized X-Ray C-arm we use, which produces the angiograms, is a floor-mounted system which offers high positioning flexibility and allows for steep angular positions to be made. This machine is capable of digital subtraction angiography (DSA) and 3D CT fusion imaging.
Patients suffering from various arterial diseases are able to get the necessary endovascular surgeries that they require. The benefits of doing an endovascular surgery (compared to open repair) under fluoroscopy (x-rays taken of a part of the body over a period of time that create a real-time video of movement of that body area) are: reduced time under general anaesthesia, elimination of the pain and trauma associated with major surgery, reduced length of stay in the hospital and reduced blood loss. Most endovascular procedures are not possible without fluoroscopy. Examples of conditions that can be treated with endovascular surgery are: Conditions of the aorta (aneurysms, occlusion), cardiovascular disorders, peripheral vascular disease, critical limb ischemia, deep vein thrombosis, varicose veins, and many other types of vascular diseases and disorders.
Is there any exciting news to share about recent technology upgrades at LHSC in your modality?
Newer imaging systems enable advanced 3-D imaging with rotational angiography, which uses a quick spin around the patient to create a computed tomography (CT) 3D image of the anatomy. This can all be done tableside in the OR. Some systems allow these images, or CT or MRI (magnetic resonance imaging) 3D images, to be overlaid or fused with the live 2D fluoroscopic images. This fusion technology is used to better guide precise stent placement.
What do you find is the most rewarding aspect of your work?
The most rewarding aspect of my work is being able to come to work every day and work with an amazing and acclaimed team.
Tracey Fratepietro, CRGS, Diagnostic Medical Sonographer (DMS) - Ultrasound
What are some unique aspects to your role in Ultrasound and how does it help with patient care?
One of the unique things about sonography is that it offers a wide range of specialties that you can experience and become proficient in. Sonographers are able to image a wide variety of organ systems, including assisting with biopsy procedures to obtain tissue samples for pathology results. On top of general and vascular scanning, our department adds such subspecialties as musculoskeletal imaging, evaluation and follow-up of transplant organs (liver, kidney, pancreas), and assisting with operating room imaging, to name a few.
Besides the skills you learn as a Sonographer, dedication to patient care is a must. Helping your patient with kind words and actions makes their experience better, and helps make the job more rewarding.
Is there any exciting news to share about recent technology upgrades at LHSC in your modality?
The Ultrasound department has new machines that offer a diagnostic tool which uses sheer wave ultrasound to evaluate for liver fibrosis. Our team has participated in the training for this new technology and will be applying it to assist the Hepatology team in diagnosing fibrotic change in the liver.
What do you find is the most rewarding aspect of your work?
I love the ability to meet, speak with and help my patients. Helping people really is the reason I decided to work in healthcare. Ultrasound examinations usually last a little longer than other imaging modalities with the sonographer and patient right beside one another for a good period of time, so we have the ability to chat and get to know each other a little!
Jason Lazar, MRT (R) (CTIC), Medical Radiation Technologist – CT
What are some unique aspects to your role in Computerized Tomography (CT) and how does it help with patient care?
As a Technologist who specializes in CT, we do scans on a wide range of patient populations and do our best to cater each exam to the patient's specific needs and requirements. We help produce a kind and caring environment for patients to help minimize procedural anxiety – especially because our machines can be intimidating. We also use various positioning techniques and aids to make patients as comfortable as possible during their scans.
In CT, we use x-rays and sophisticated software to produce three-dimensional (3D) images which can be rendered into many different angles or even 3D models. We also insert IVs and administer contrast dye using a power injector to help enhance certain anatomy for imaging during some exams.
Is there any exciting news to share about recent technology upgrades at LHSC in your modality?
We are excited to have some of the newest CT scanners and associated applications right now. These new scanners are capable of producing highly detailed images with the ability to also decrease patient dose by a substantial amount compared to previous generations of technology.
What do you find is the most rewarding aspect of your work?
I believe the most rewarding aspect of being a CT Technologist is knowing you did your best to help patients each day.
Johnathon MacLennan, MRT (NM), Medical Radiation Technologist - Nuclear Medicine
What are some unique aspects to your role in Nuclear Medicine and how does it help with patient care?
We can detect minute changes in physiology allowing us to detect disease in its earliest stages or target treatment to specific areas (theranostics) and monitor the response to treatment. The technology works the opposite to x-ray (where the image is captured by looking through the body). In Nuclear Medicine, the image is captured after injecting the radiation into the body and the emissions from the radiation are viewed.
The radiation that we primarily work with is from the decay of radioactive isotopes. This decay produces gamma-rays that are detected by a special scanner (gamma camera) and converted into an electrical signal that can be used to create a digital image.
Nuclear medicine technologists are experts in all aspects of preparation, quality control, safe handling, administration, and disposal of radiopharmaceuticals. In addition to operating our imaging systems, we also use specialized radiation detection equipment for dose calibration, blood sample measurements and radiation monitoring.
Is there any exciting news to share about recent technology upgrades at LHSC in your modality?
I am very excited to use the newly installed PET/CT (Positron Emission Tomography/Computed Tomography) which will be able to detect cancer at the molecular level. This will be an important tool in therapy planning. This is cutting edge technology with many other uses that I can’t wait to explore.
What do you find is the most rewarding aspect of your work?
The most rewarding aspect of my work is the satisfaction of knowing I am helping my patients in a unique way.
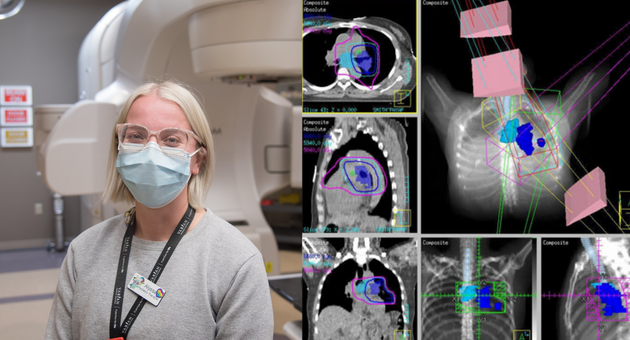
Alyssa Moniz, MRT (T), Radiation Therapist – Radiation Therapy
What are some unique aspects to your role in Radiation Therapy and how does it help with patient care?
The Radiation Therapist role looks like a lot of physics, science and math, but it encompasses patient care as well. We see patients daily and address any concerns, side effects, or problems that arise during treatment. Whether it be physical or emotional, we try our best to make the experience easier for patients. We make a lot of on-the-spot decisions when imaging our patients and we have to be quick on our feet, able to assess our images quickly and efficiently (whether it be an X-Ray or CT scan). We take a variety of images, depending on the site and the plan to treat the patient. This can include Gated CTs – which only capture the image during the exhalation phase of the patient's breathing cycle.
Is there any exciting news to share about recent technology upgrades at LHSC in your modality?
We recently acquired two new Canon CT scanners for planning that offer new functionality. Also, we have recently received a PET CT scanner, which is more sensitive than an ordinary CT scan.
What do you find is the most rewarding aspect of your work?
The most rewarding part of my job is having that bond with my patients, and seeing them finish treatment with a smile on their face. It's nice that we can take something so scary and foreign to them, and give them comfort and courage to take on their journey in the fight against cancer.
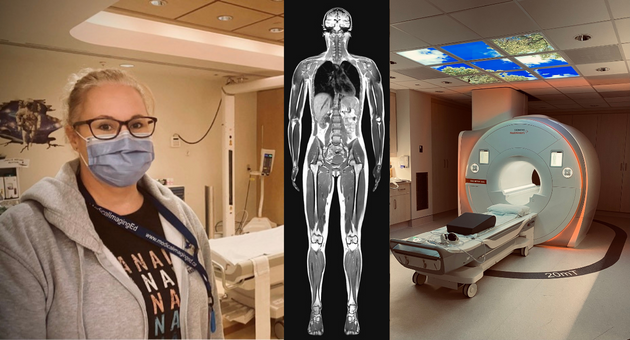
Krista Pare, MRT (MR), Senior MRT - MRI
What are some unique aspects to your role in MRI and how does it help with patient care?
There is a significant safety factor in MRI (Magnetic Resonance Imaging) because we deal with multiple energy forms. We are dealing with a strong magnetic field that poses risks for metal projectiles, danger to patients with certain implants and many other safety concerns. No one patient is the same, so we are constantly looking to eliminate associated risks for each individual case.
Like all imaging modalities, our goals are to help with diagnosis. We work alongside teams in the London Regional Cancer Program (LRCP) by doing scans that they fuse with CT to help them pinpoint exact locations for radiation therapy.
We can also help our pregnant populations since we don’t use ionizing radiation – our scans are safe for them to undergo. We even scan fetuses as well.
Is there any exciting news to share about recent research at LHSC in your modality?
There is an fMRI in paediatrics for epilepsy (the f stands for functional). While we scan their brain, they will watch and perform a few tasks. For example, they will see an image appear on their video google (like a watch or dog) and they will say or think what the image is. This task will cause a certain part of the brain to respond. Another task is to squeeze or raise their hand on the same side they see the image. Again, this causes a different part of the brain to respond. The research team gathers thousands of images and can determine what parts of the brain are functioning and avoid those areas during surgeries to help stop the seizures the patients are having.
What do you find is the most rewarding aspect of your work?
The ability to gain the trust of our paediatric patients and have them complete a successful MRI with no sedation/anesthesia required is an aspect of my work that I find rewarding. The proud look on the child and their parents faces never gets old as well as the cheers and rewards they receive by all staff involved!