
London Health Sciences Centre (LHSC) is celebrating our 2023 Patient Safety Champion Awards recipients. The recipients received their awards at an annual ceremony that recognizes members of Team LHSC who have demonstrated a passion for and commitment to improving patient safety.
“LHSC has a long, proud history of prioritizing patient safety. Patients are at the centre of everything we do, and we take our responsibility to provide them with safe, high-quality care very seriously,” says Tammy Quigley, LHSC’s System Innovation and Business Development Executive.
“Each year, we work tirelessly to introduce new formal and informal patient safety initiatives across the organization, and these awards are an opportunity to recognize some of these initiatives,” she adds.
Individual Award: Kim Madsen
The Individual Award celebrates an individual on Team LHSC who embeds all patient safety best practices in their daily work and continually looks for ways to raise the bar in service of our patients.
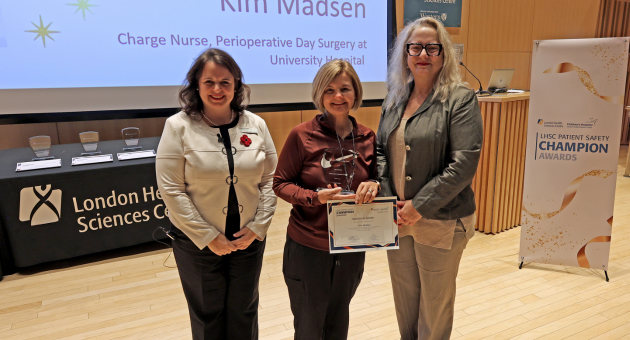
Kim Madsen has been a Registered Nurse at LHSC for over 35 years. She currently works as a Charge Nurse in Perioperative Day Surgery at University Hospital, where she preps patients admitted for elective, pre-booked surgeries.
Madsen’s colleagues describe her as a forward-thinker who is always anticipating and mitigating potential risks. For example, while getting patients ready for their procedures, Madsen helps ensure all orders and checklists are done prior to the patient arriving at the operating room and makes sure any potential concerns are brought to light early enough to be addressed without causing delays.
“I never take a patient’s safety for granted,” says Madsen. “The protocols are there for a reason and should never be seen as an inconvenience or hinderance to the process.”
Madsen was at work when she received a call from Tammy Quigley saying she’d be receiving this year’s Individual award.
“It was a really nice surprise because I didn’t know I was nominated,” says Madsen. “But patient safety is truly a team effort. Everyone on the periop team strives to provide patients with the safest possible surgical experience.”
“We’re their biggest advocates” she adds.
Leader Award: Sherry Szucsko-Bedard
The Leader Award celebrates a formal leader at LHSC who spearheads patient safety initiatives and client inspires their team to do the same.

Sherry Szucsko-Bedard has been part of Team LHSC for more than 34 years. Currently the Operations Manager for Inpatient Surgery at University Hospital, she accepted a casual position in medicine as a new grad before moving into a full-time role in the transplant unit. It was here she honed her clinical skills before moving into risk management and then back to a clinical role.
During her more than three decades on staff, Szucsko-Bedard has led and been part of many patient safety projects. She says her passion for them was born early in her career.
“I had an epiphany one day when I realized, 'Oh my goodness, this could be my mother or grandmother, and if it was them, how would I want them to be treated?'” she says. “I see my loved ones in each patient I care for, and this has stayed with me regardless of who the patient is or what unit they’re on.”
At the end of the day, Szucsko-Bedard says she feels lucky to be surrounded by such a caring and supportive team that is truly embracing LHSC’s Continuous Improvement of Care (CIC) initiatives. Since the spring of 2023, they have completed more than 94 of them.
From bringing in new patient lifts to advocating for additional crash carts, she says it’s all about being proactive.
“I’m so honored and humbled to receive the Leader award, but this isn’t just for me, it’s for my whole team. They bring their concerns to me, and I carry them forward. We truly champion this work together.”
Team Award: Thoracic Remote Monitoring Team
The Team Award celebrates a team at LHSC that has implemented an evidence-informed quality improvement project that has improved outcomes for patient safety.

Dr. Richard Malthaner, Dr. Mahesh Nagappa, Angeline Sloan, Natasha Wood and Nida Fatima are known as the Thoracic Remote Monitoring Team. Together, they leverage technology to reduce the number of patients who present at Victoria Hospital’s emergency department (ED) after being discharged post-surgery.
What started as a pilot project titled, “Digital Home Monitoring to Improve Postoperative Outcomes After Thoracic Surgery” has turned into a robust hybrid-style clinic that sees about 25-30 patients each month. So far, it has improved access to care and decreased ED admissions and flow delays.
“We know that about 20 to 30 per cent of patients who undergo thoracic surgeries such as lobectomies and esophagectomies typically present back to the ED within 30 days,” says Dr. Richard Malthaner, LHSC’s Chair of Thoracic Surgery. “In most cases, the issues are minor, but all have the potential to become life-threatening if not addressed early. We needed to come up with a solution that would allow us to intervene before the ED is needed.”
Patients who consented to participate in the clinical study were randomly assigned to receive only in-person care or the home monitoring of vital signs like oxygen and blood pressure. Those in the remote monitoring group received automatic reminders to check their vitals at certain times of day and the remote monitoring team was able to see the data in real time. The study found that ED visits were reduced and adverse events prevented. Patients were also extremely satisfied, so the program continues.
Natasha Wood, Registered Nurse, proactively follows up with each patient via telephone or video call within 24 hours of their discharge to see if they have any questions or concerns. She also works with them to set up a check-in schedule for the days and weeks ahead and explains how they can get a hold of the team if anything changes in the meantime.
“It’s all about what the patient is most comfortable with,” says Wood. “Some patients opt to have me check in with them daily, while others opt for weekly or less, depending on where they’re at in their recovery process.”
At their check-ins, Natasha provides solutions to issues like pain and wound care concerns, and will escalate the patient back to the physicians, if need be.
“The number of patients who need to be followed up with in person is much lower than those who can be seen virtually, which is why this model works,” says Dr. Malthaner. “It ultimately allows our patients to receive the high-quality care they’re used to, but in a more convenient and accessible way.”
“Home is also safest,” adds Angeline Sloan, Clinical Nurse Manager, who oversees the clinic’s operations. “Patients benefit from the sense of normalcy they don’t get in the hospital, where there’s also frequent sleep interruptions and an increased risk of infection.”
The team chose to test their remote monitoring model with thoracic surgery patients because they typically require the most care after discharge, but hopes to expand it to other surgical pathways in the future.
“Sending someone home to be monitored is a delicate balance between privacy, confidentiality, and safety. What we’re currently doing is ‘safe’ from each of these perspectives and we must keep it that way with however we move forward,” says Dr. Malthaner.
The idea came to fruition in early 2020 when the team pitched it to LHSC’s Medical Affairs department. They were told that if they could produce favourable results, the funding would continue. Unsurprisingly, most patients “agree” or “strongly agree” that they would recommend the remote monitoring program to future patients, and the funding is now renewable on an annual basis.
“I'm so happy for our team and what we’ve accomplished for our patients,” says Dr. Mahesh Nagappa, Anesthesiologist. “Winning the Team award has really boosted our morale and encouraged us to keep going.”
Physician Award: Dr. Uday Deotare
The Physician Award celebrates a physician or resident at LHSC who has demonstrated a passion for and commitment to patient safety from a physician’s perspective.
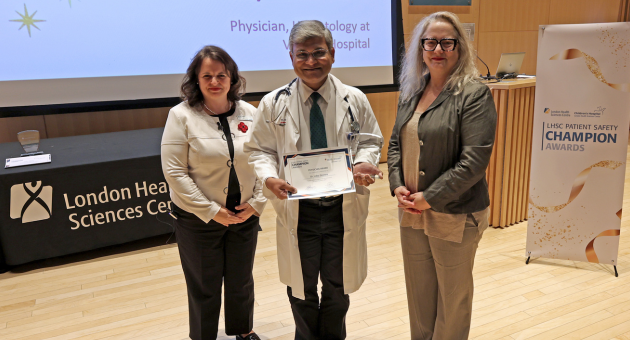
Dr. Uday Deotare is the physician lead for the C7 Inpatient Unit Improvement Team. He also serves in LHSC's Blood and Marrow Transplant Program and on its Quality Committee.
Dr. Deotare developed an interest in quality improvement during his fellowship and went on to complete his Master of Health Care Quality. He joined LHSC in 2017 and immediately began looking for ways to put this formal education to use. Since then, he has played a leading role in numerous patient safety-related initiatives.
These initiatives include encouraging stem cell transplant recipients to re-do their vaccinations so they can recover protection after transplantation, safe transition of autologous transplant inpatients to outpatients, and helping home care nurses reduce medication errors.
Most recently, he and the Unit Improvement Team designed and executed the “Choosing Wisely: Reducing Bloodwork” inpatient study, which is aimed at optimizing and reducing unnecessary bloodwork for autologous stem cell transplant patients.
“When a patient is admitted, automated bloodwork orders are put in,” explains Dr. Deotare. “And taking more blood volume than is absolutely necessary from a patient can result in hematology concerns because they’re often already anemic, and the more blood you draw, the lower their hemoglobin gets. This leads to more bloodwork needing to be done and then suddenly you're stuck in a vicious cycle.”
But the benefits of drawing less blood go even further than that. It can also reduce blood test related costs and allow patients to feel less discomfort and disruption throughout the day, says Dr. Deotare, who was excited to learn he was the recipient of this year’s Physician award.
“Patient safety and quality improvement are near and dear to me,” he says. “So, this was a recognition of everything I had been working towards, but even more so, it was a recognition of what our team had been working towards. It feels good to know the work we do is noticed and appreciated.”
Patient Partner Award: Anne Leishman
The Patient Partner Award celebrates the significant role a Patient Partner has played in the development or advocacy of various patient safety initiatives at LHSC.

Anne Leishman has been a Patient Partner at LHSC for the past four years. She has also been a Patient Family Advisor with the London Regional Cancer Program (LRCP) since 2015, and prior to this, was a long-time volunteer at LRCP through the Canadian Cancer Society.
Her journey as a Patient Partner began when she got an email saying LHSC was looking to incorporate the patient’s perspective in some quality improvement work.
“I was immediately like, ‘I can do that!’” says Leishman.
Since signing up, Leishman has become a valuable member of the Quality and Patient Safety Council, Patient Experience Advisory Council, Patient and Family Advisory Council and Fall Prevention and Care Partner Presence Committees.
She was also part of the Rapid Response Team formed at the beginning of the COVID-19 pandemic.
“Policies needed to evolve quickly as the pandemic was declared, and part of my job was to advise on caregiver presence rules, screening at entrances, masking and more,” says Leishman, who also helped to expand the virtual care program at a time when limiting the number of people gathered in a physical space was a top priority.
“I would get calls and emails about things that needed to be reviewed by the end of the day, and I was always more than happy to do it,” says Leishman. “It was important, and I took it seriously because I knew it was impacting a lot of lives.”
These days, Leishman says she’s probably doing some sort of volunteering for the hospital at least once a week.
She was surprised to receive a call from Tammy Quigley saying she won the Patient Parter award because she didn’t know she had even been nominated, but says she feels “profoundly grateful.”
“I feel like I’m accepting this award for all of us Patient Partners,” Leishman says. “We work together to provide input and are happy to do so because we know what we have to say is valued.”
“Regardless of what committee or meeting I have been in, I have always felt welcomed, included and heard,” adds Leishman.