November 14, 2022
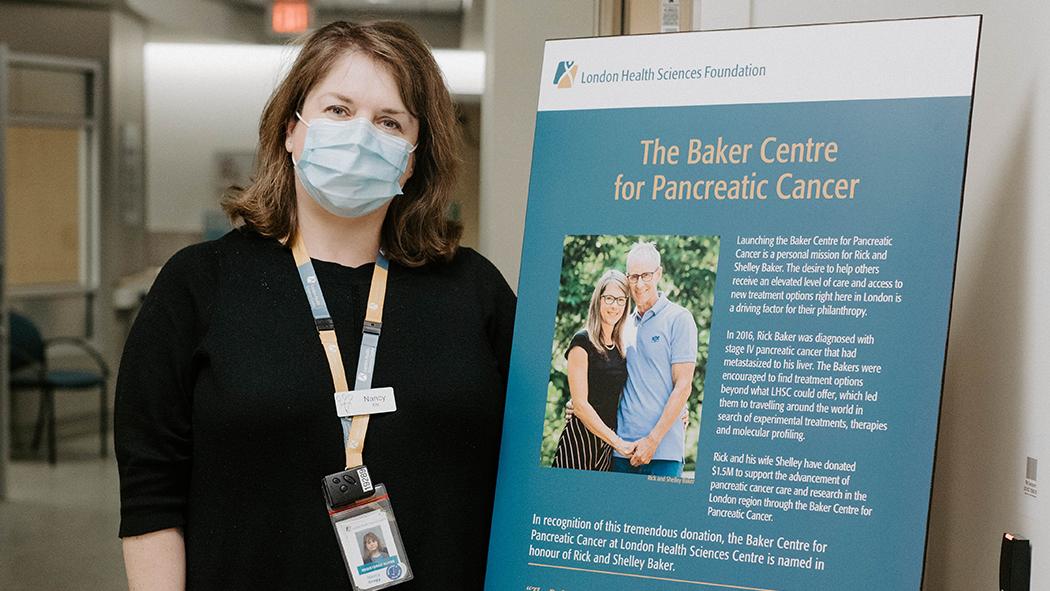
The Baker Centre for Pancreatic Cancer at London Health Sciences Centre (LHSC) opened in 2019. The Baker Centre was created from the vision of Rick and Shelley Baker who donated $1.5 million to support pancreatic cancer care and research in the London area. This donation, and the subsequent opening of The Baker Centre has made a significant impact on pancreatic cancer patients’ access to specialized care.
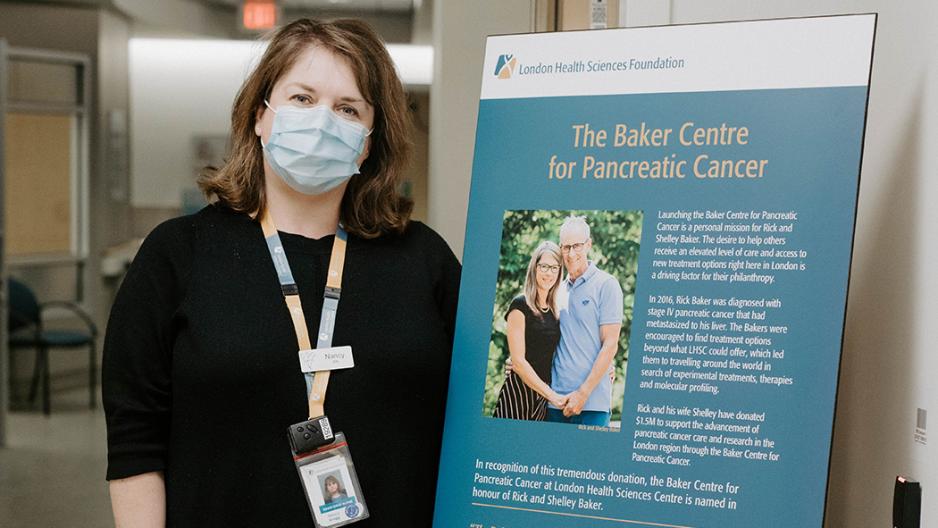
In recognition of Pancreatic Cancer Awareness Month, we want to highlight the path a patient takes through The Baker Centre to help demystify the experience prior to the visit. Nancy Gregg, Patient Health Facilitator for The Baker Centre outlines the steps a person takes as a patient of The Baker Centre.
How does a person become a patient of The Baker Centre?
Nancy Gregg: A person becomes a patient either from an internal referral from a surgeon at LHSC or from a referral in the community – which includes the south west region and beyond.
After a person becomes a patient, what comes next?
NG: Once a patient has been scheduled for their first appointment, I contact the patient by telephone and gather health and social information for their intake and explain what their first appointment is all about – who they’ll meet, how long the appointment will be and answer any questions they may have prior to their appointment. I also provide my contact information at this time so the patient and family are aware there is someone to call if needed.
What is involved in that first appointment?
NG: The first appointment can be lengthy – often two to three hours long. The patient sees the multidisciplinary team at this first appointment. This first meeting is a comprehensive, informative and often decision-making appointment.
The patient visits The Baker Centre which is currently located on the third floor of the London Regional Cancer Program (LRCP). The patient will meet with the primary nurse and then be seen by the multidisciplinary team (Medical Oncologist, Surgical Oncologist and sometimes the patient will also meet the Radiation Oncologist). The patient will also meet members of the team who work in health disciplines that can assist them during their time as a patient of The Baker Centre such as the dietitian, social worker and our clinical research team.
At this appointment, patients will also get their blood taken for tests and will learn about the various clinical trials they may be eligible to participate in. They will learn more about those clinical trials before they make the decision to participate in these important pancreatic cancer research projects. This is a part of the decision-making process patients make during the first appointment
After the patient has met with everyone, the plan (or next step) is outlined to the patient. At this point in the appointment, I go in and sit with the patient and family to ensure they understood everything and that they have my contact information in case they have any questions moving forward.
After this initial appointment – which usually happens on a Monday – I call the patient two days later to re-connect and ask if they have any new questions or concerns. I, again, ensure they have my contact information at the end of that call. I am the main contact person for every pancreatic patient at The Baker Centre to help them navigate their cancer care journey.
What usually follows the initial appointment?
NG: During that first appointment is when their treatment plan will be decided, and it depends on the individual patient on what their next steps are. They may be sent for more testing, biopsies, scans or other imaging. Some may choose supportive care only – meaning they move forward without treatment and instead focus on quality of life.
Regardless, at the end of the first appointment they will go away with a plan and know where they’re heading after the initial appointment.
If patients move on to receive treatment, are they still considered a patient of The Baker Centre?
NG: Yes. Whether a patient receives chemotherapy or radiation therapy or surgery or a mixture of those treatments from other areas within the London Regional Cancer Program (LRCP) at LHSC, I am still the main contact that helps patients of The Baker Centre navigate their care.
The only patients I don’t continually follow are the patients who choose supportive care only. I ensure those patients are being cared for by a palliative care team. I am still available to those patients if they have questions or concerns about their supportive care process, I simply don’t follow them as closely as the patients who continue with treatment because the palliative care team becomes their primary contact and resource.
What are some other practices of The Baker Centre that patients should be aware of?
NG: We want patients to know that with the unique aspects of pancreatic cancer, we work hard to ensure patients are seen as quickly as possible after the referral is received. Time is of the essence in cancer care, but especially with pancreatic cancer.
My role is rather unique as well. I act as the main, direct contact for patients of The Baker Centre for any questions, concerns or comments they want to share. Each patient has my direct extension and I travel with them through their entire experience as a patient of The Baker Centre.
The Baker Centre team keeps the lines of communication open between one another and between other teams so we know who is doing what at what time. We are very connected and this helps in delivering excellent patient care.