LHSC 150: The hospital pharmacy

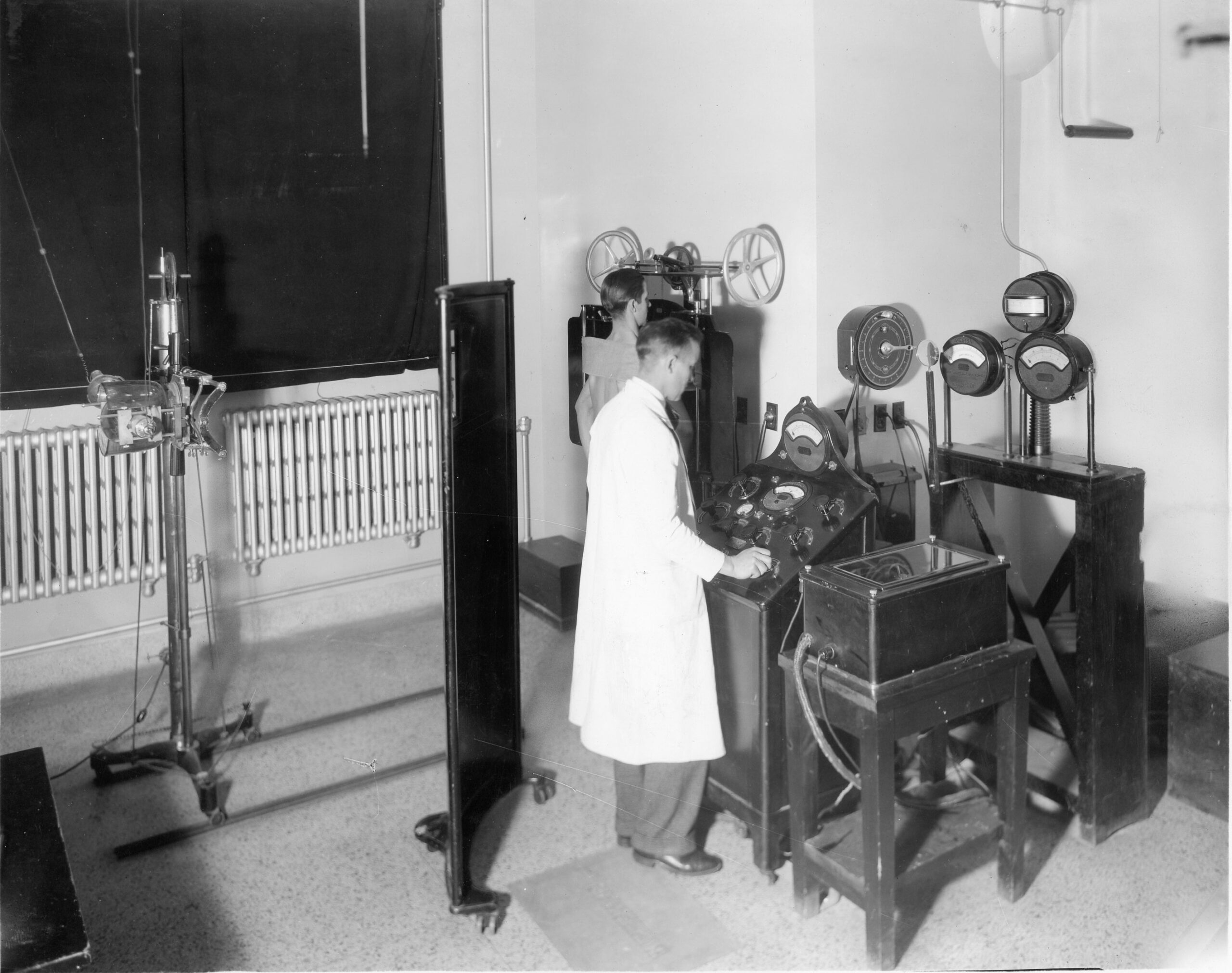
Above: The dispensary at Victoria Hospital, circa 1910.
As London Health Sciences Centre (LHSC) celebrates 150 years of great care, teaching, and research, we look at how the Pharmacy team has evolved within the hospital setting.
From the primary function in the early 1900s of preparing and dispensing medications, the Pharmacy team are valued members of the health-care team, sharing their expertise and knowledge of medications, dosages, potential interactions and antimicrobial stewardship with colleagues and patients. A heavily regulated profession since the 1990s, these professionals provide lifesaving and life-improving medications to inpatients, outpatients and the community.

LHSC’s Pharmacy team has provided care to both inpatients and outpatients for more than 75 years. Between 1941 and 1951, pharmacists filled 46,116 prescriptions for inpatients and 103,740 prescriptions for clinics or outpatients. Fast forward to 2024, and the team of 300 members dispensed over nine million medication doses to admitted patients, processed over 160,000 prescriptions for staff and outpatients, and reviewed 2.4 million medication orders.
From the floor – University Hospital
Tara Lyons Cork is a retired pharmacist from University Hospital who began working in the Intensive Care Unit in 1987 and spent the last 20 years in General Surgery. Lyons Cork still supports the team on a part-time basis. Unlike her predecessors from 1950s who provided support from within the Pharmacy’s physical location, Lyons Cork works on the floor directly supporting patients, nurses and physicians.

The biggest change she has witnessed over the past three decades has been the advances in electronic health records.
“When I first started, orders were paper-based copies and there was an increase in lag time and turnaround time for assessment,” says Lyons Cork. “You used to have to review and assess the prescriptions without knowing all the details of the patient, such as kidney function levels. Today things come in quickly and we have access to updated patient specific information for reviewing prescriptions.”
Lyons Cork has been involved with these changes throughout her career working through software changes and Y2K. A passion of hers, she worked directly with the digital advancements in patient records and continues to enjoy sharing this knowledge and experience with new staff.
From the floor – Victoria Hospital
Lynne Kelly started working in the Critical Care and Trauma Centre (CCTC) at South Street in 1992 and is now at Victoria Hospital. Like Lyons Cork, Kelly has also witnessed massive changes in technology with respect to the dispensing of medications. It has shifted from a very manual process to one that uses a highly sophisticated robot.
Kelly also notes some of the physical changes that have occurred in pharmacy over the years. The sterile room, for example, has changed from one where people could smoke while preparing medications to one that is a clean room complete with hoods and pressured air.
During her early years with LHSC, Kelly had the opportunity to help plan the move of the medication rooms in the CCTC from South Street to the new location on Commissioners Road.
“It was hugely exciting,” says Kelly. “We were moving from a very old building with a lot of character to a brand new CCTC unit with big, beautiful clean spaces where everything was new and state of the art.”
The bed space in the CCTC unit is one example Kelly gives reflecting the size of the space, which went from being roughly 75 sq/feet per bed to 225 sq/feet per bed.
“We were also no longer using tape on the floor to demarcate the infection zone,” she recalls. “It was a cool experience to be a part of and the CCTC team was really collaborative, giving Pharmacists our own space within the unit.”
“The job itself of ensuring we provide the right medications based on patient needs hasn’t changed, but the tools have,” reflects Kelly. “Literature reviews used to be done over days by hand using books from the library, now we have the internet search engines and we can get the information quickly.”
Snapshot of Pharmacy Services through time
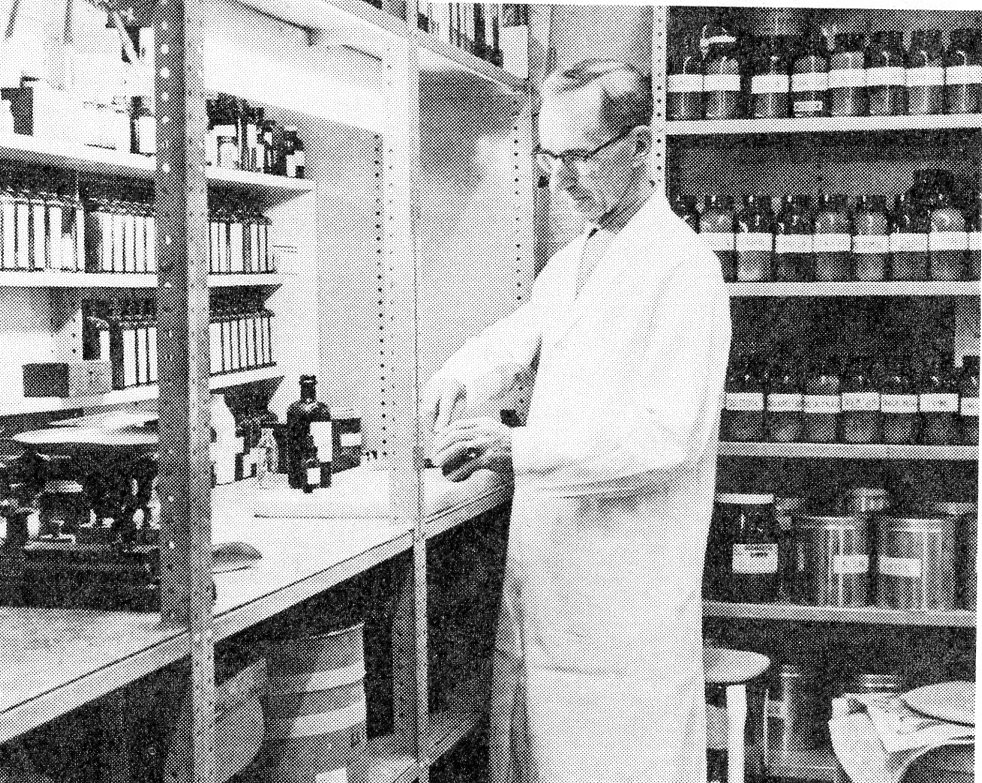
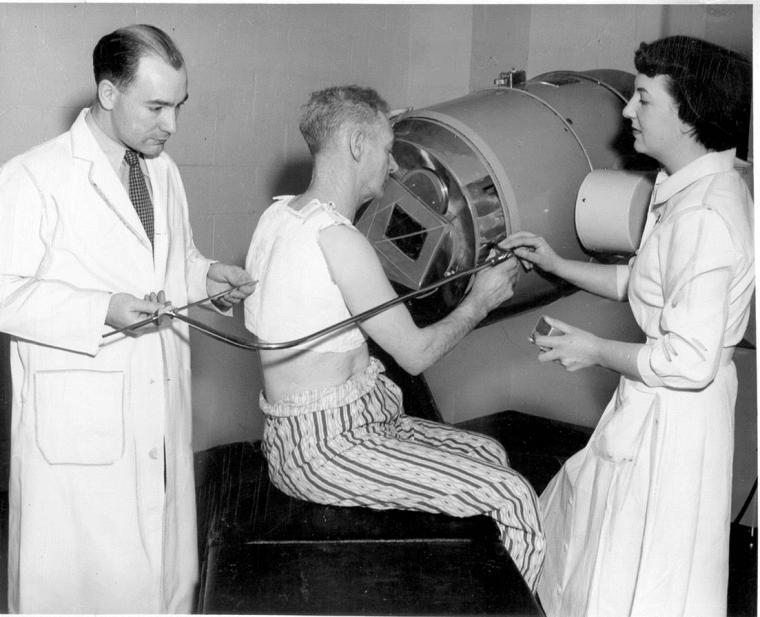
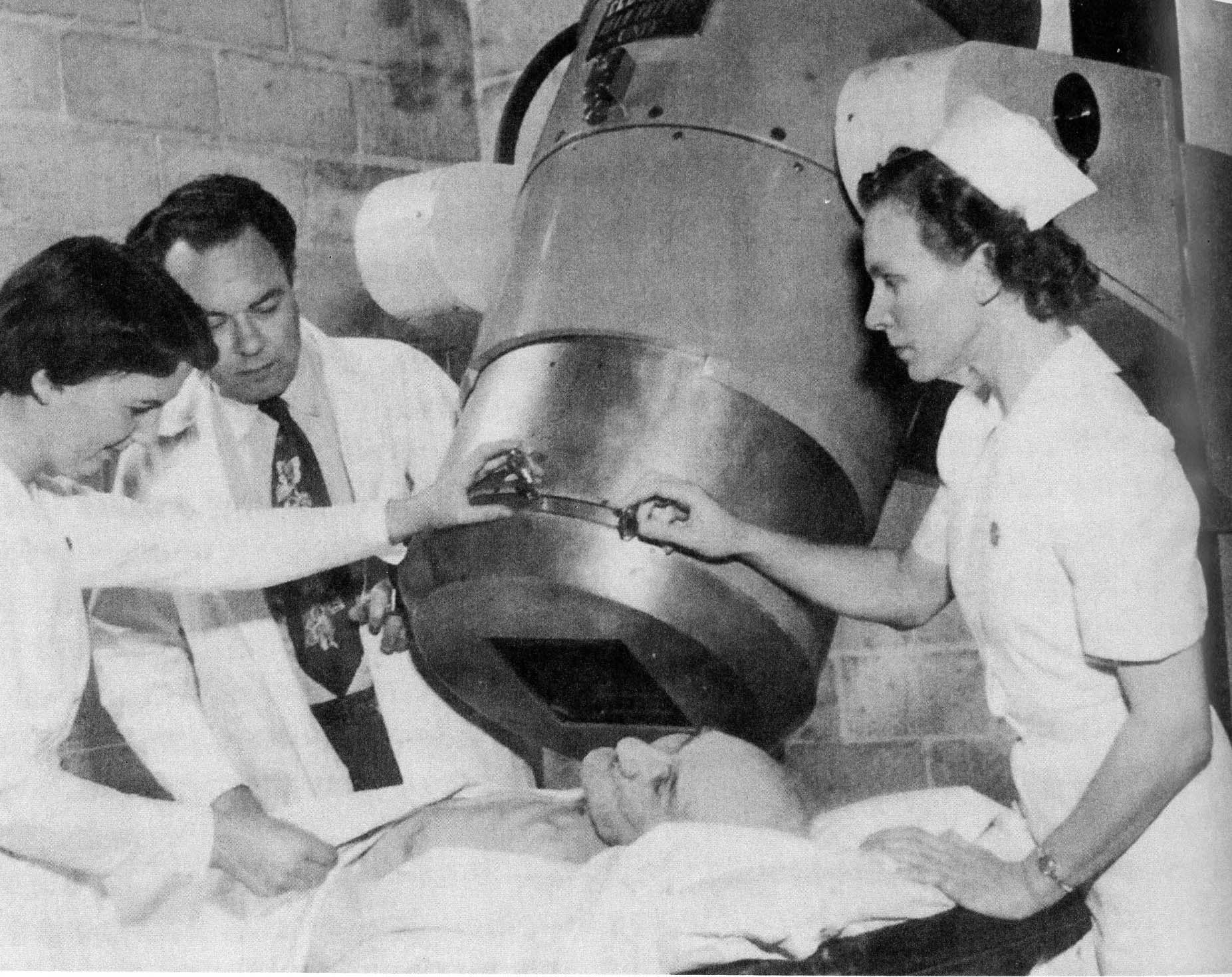
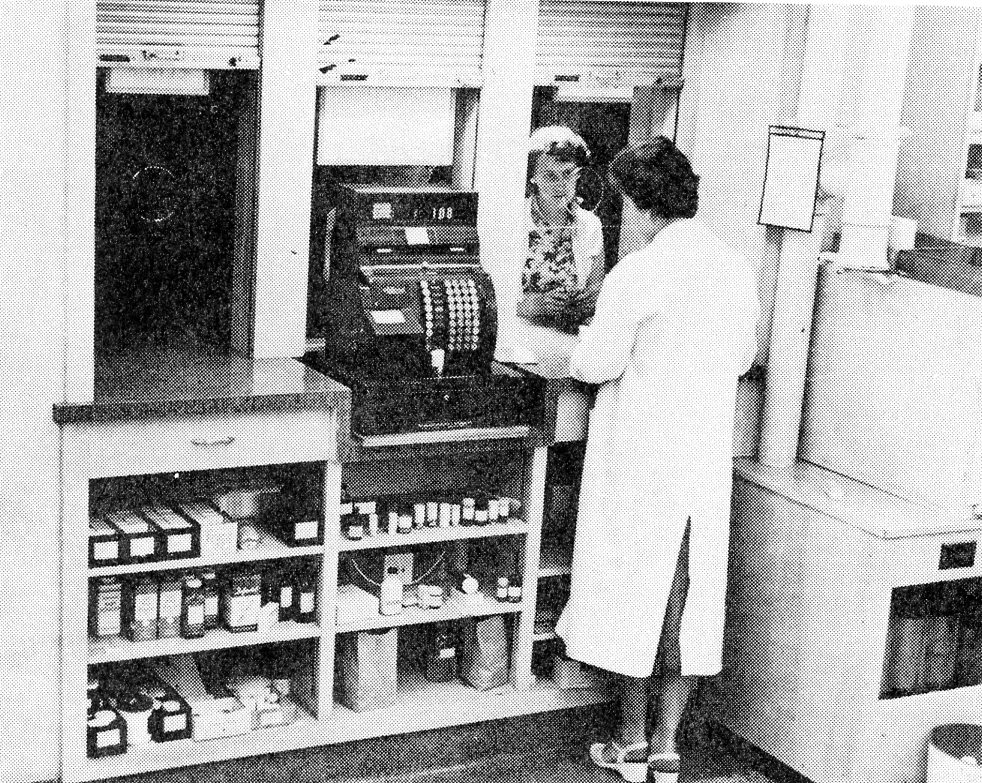
In 1958 the Pharmacy at Victoria Hospital was renovated to include open shelving for easier access of medications, inclusion of an electric stove and an electric mixing machine in the compounding area to speed up operations, and a unique infra-red bottle drying machine. Additionally, they had five individual dispensing areas, each equipped with typewriters, a manufacturing or compounding area, and an area designed for the preparation of inpatient stock.
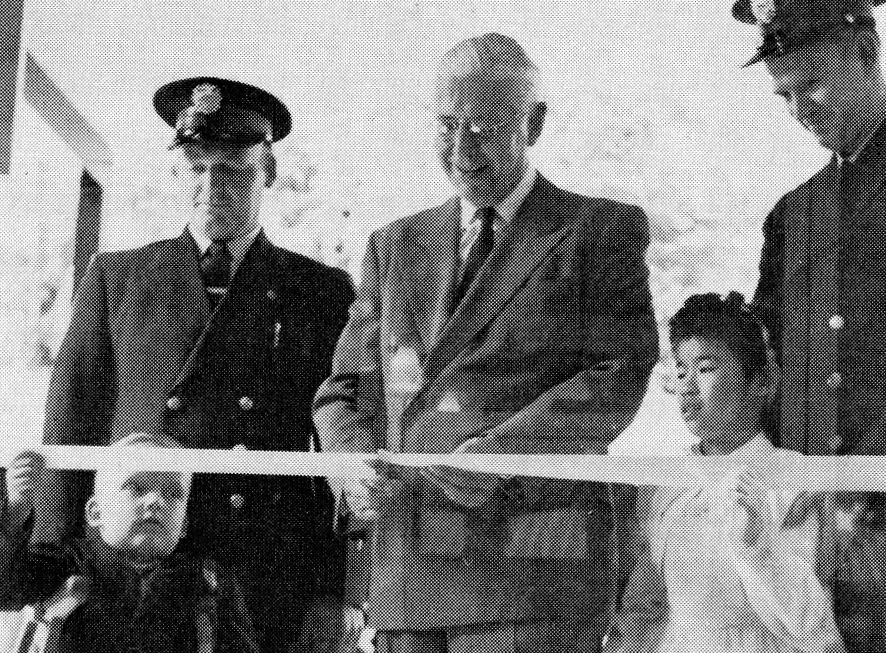
In the late 1960s early 1970s, changes in legislation facilitated the expansion of the role of the pharmacy within hospitals. To meet this increased workload, new patient medication dispensing techniques have been devised to provide better patient care, greater human resources, productivity, and improved utilization of hospital pharmacy space. Victoria Hospital was the first pharmacy in the country to implement a ‘sectored pharmacy.’ which divided the pharmacy into workflow specific areas including inpatient dispensing, outpatient dispensing, narcotic control, and assembly.
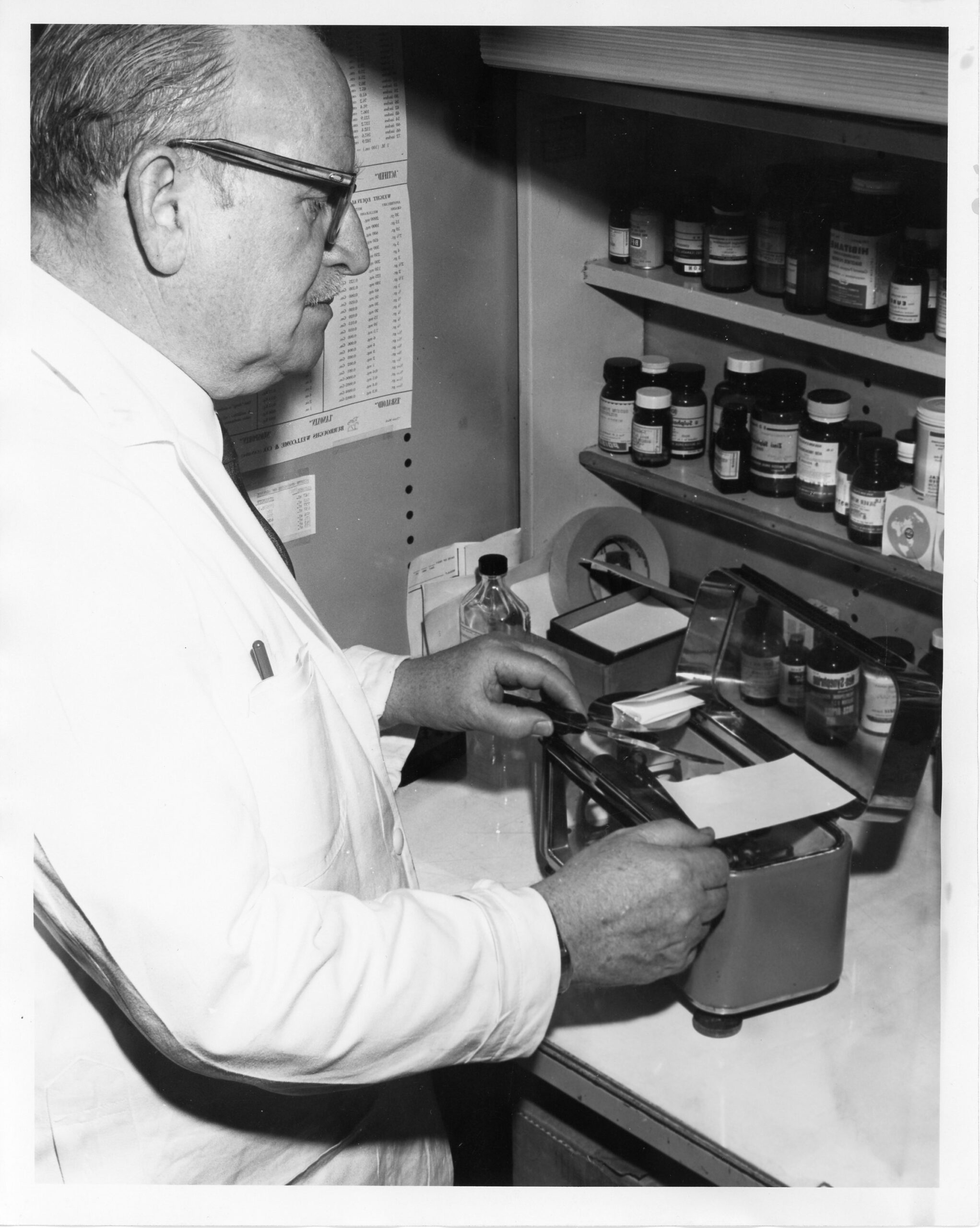
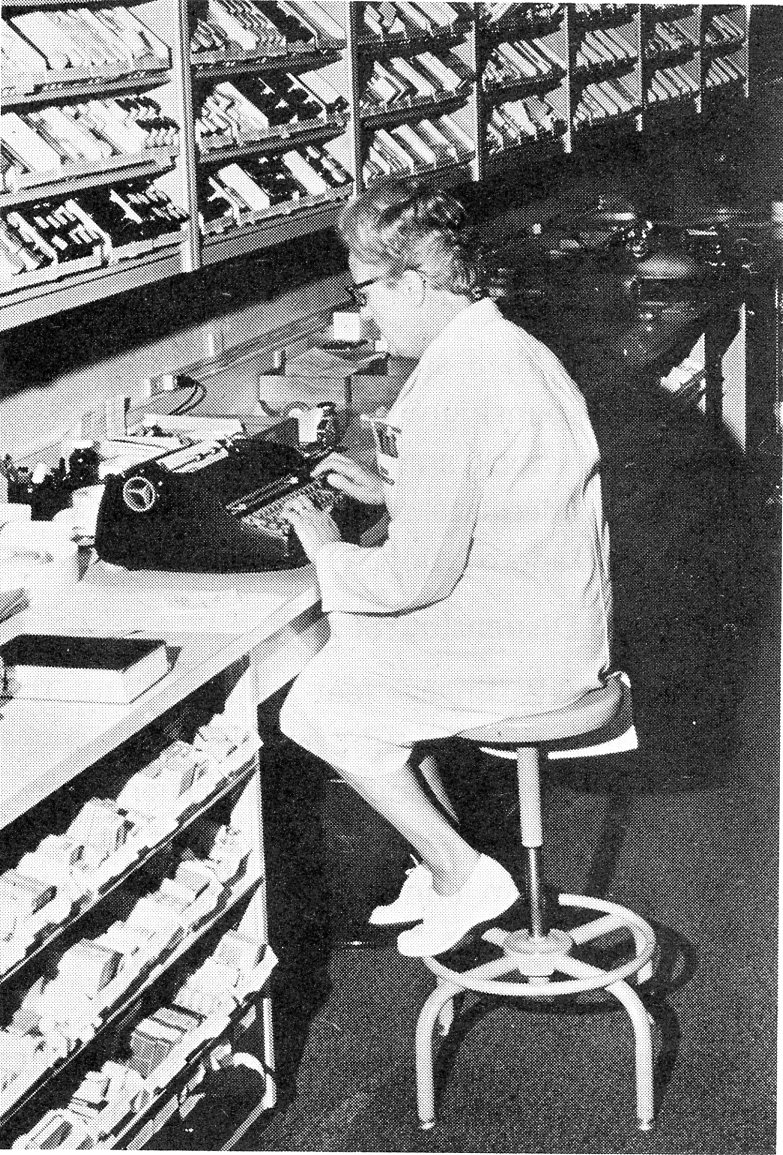
Additional advancements during this time included an automatic tablet counter, printing equipment, typewriters, and laboratory and pharmaceutical equipment to help work be done more accurately and rapidly.
“Pharmacy is the science and art of those matters related to the procurement, preparation, control and distribution of drugs including the numerous elements that comprise these entities,” according to an article titled “New concept in Pharmacy Services”, in Vic Life June 1970, author unknown.

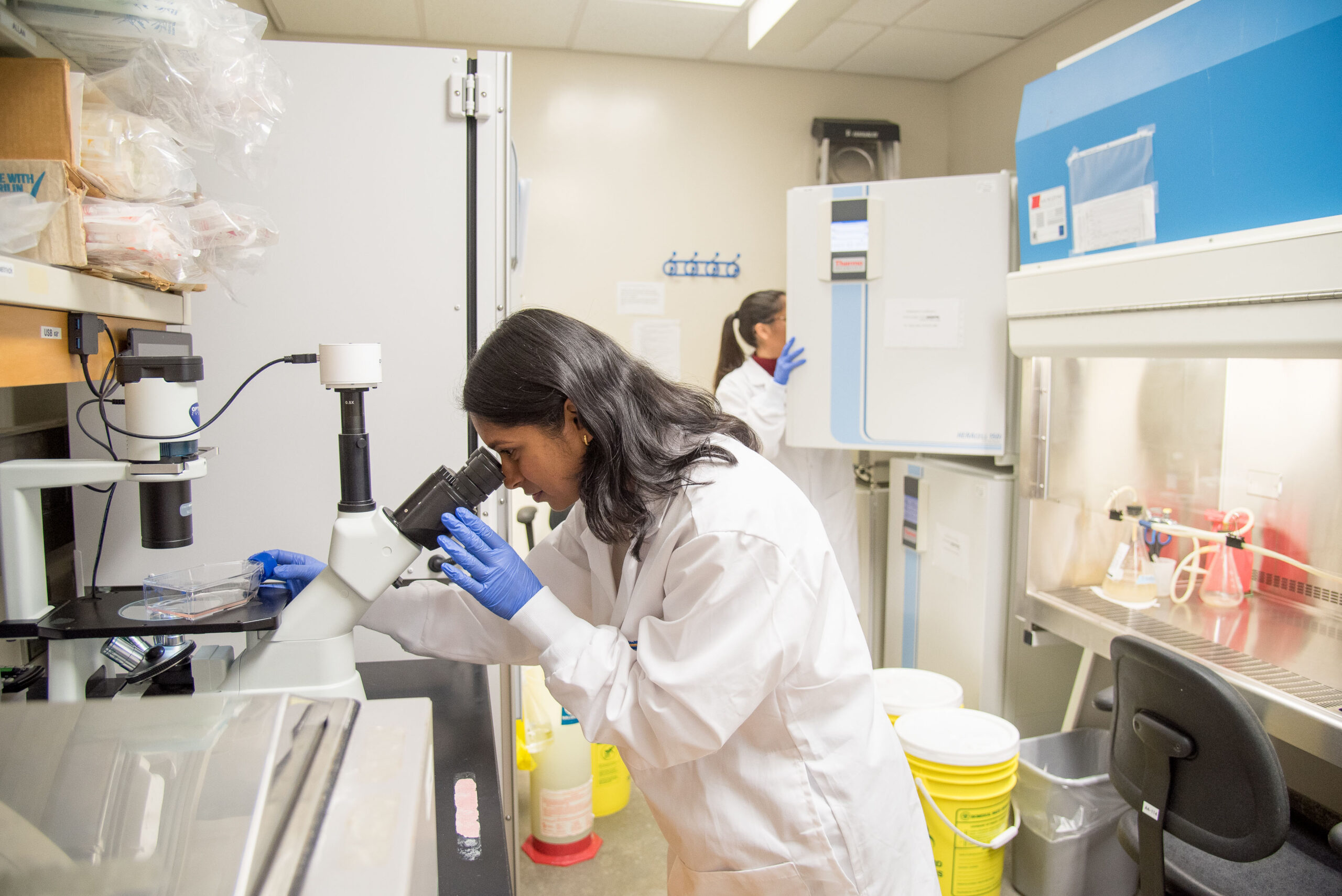
Alex Wyatt, Pharmacy Technician at LHSC prepares to send a medication packet put together by the PillPick machine to an inpatient unit in 2023.
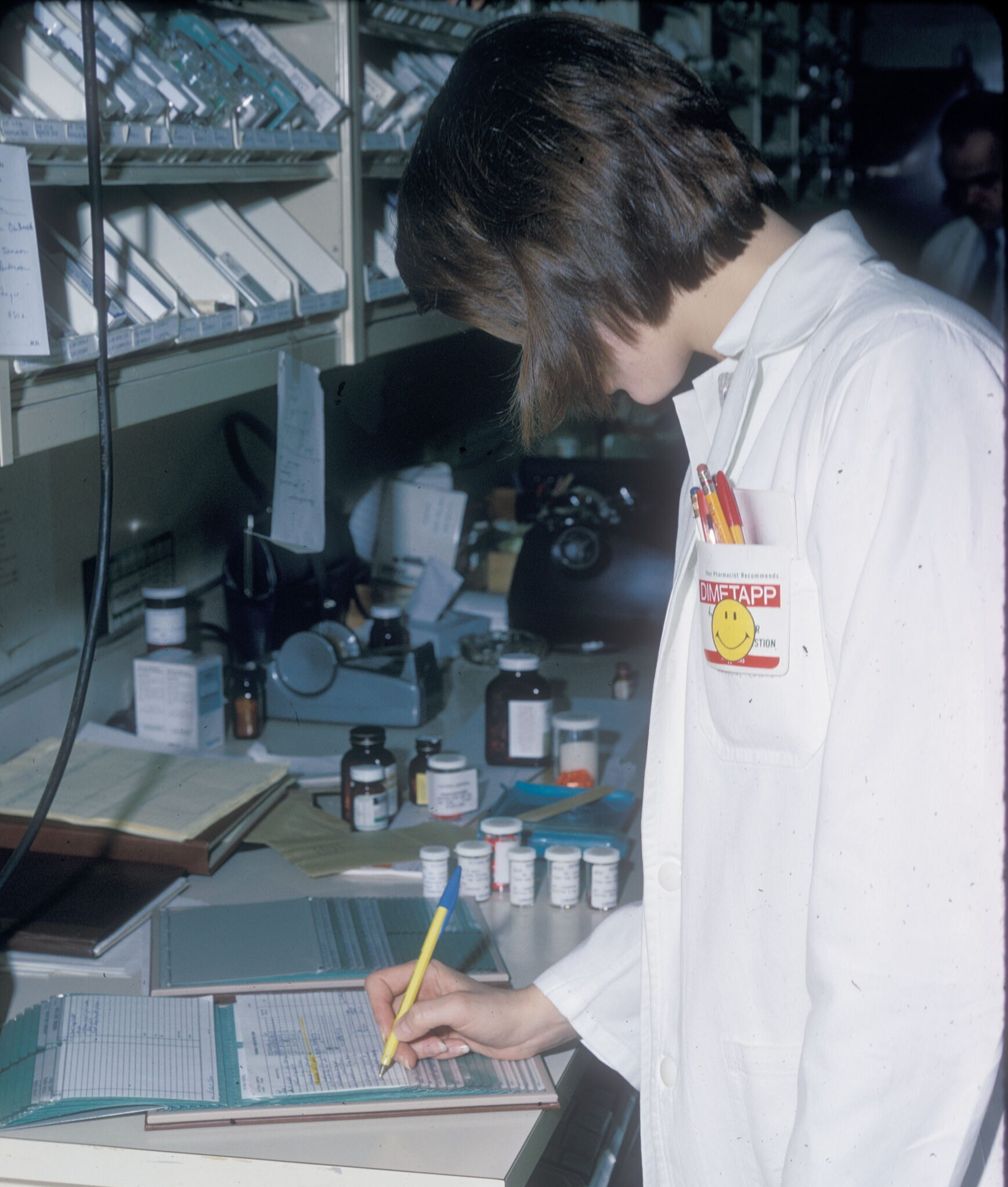
Claudia Hildebrant, a pharmacy technician at LHSC’s University Hospital works behind the scenes to prepare medications for distribution to various inpatients across the organization in 2025.