The history of cancer care at LHSC is a history of innovation
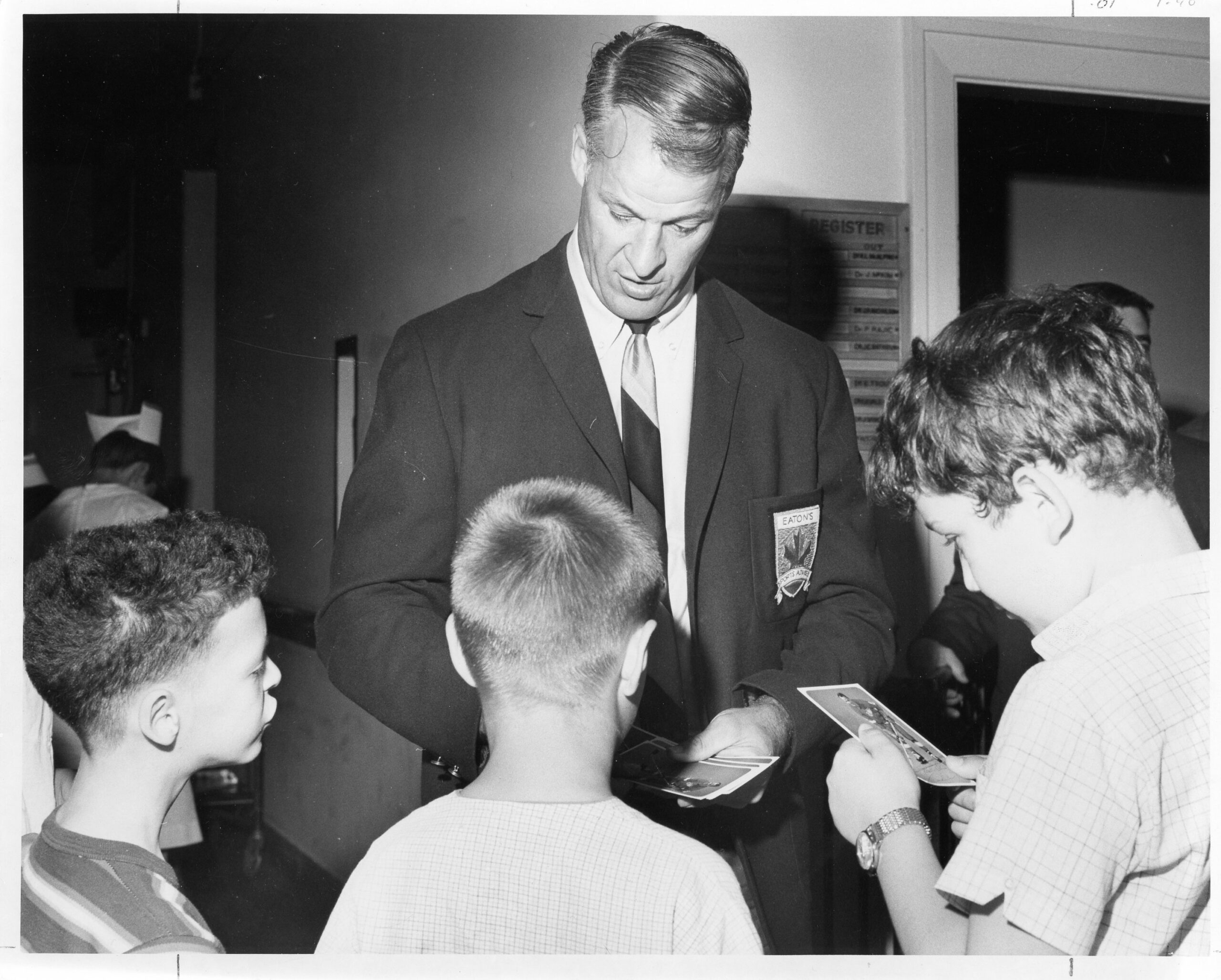
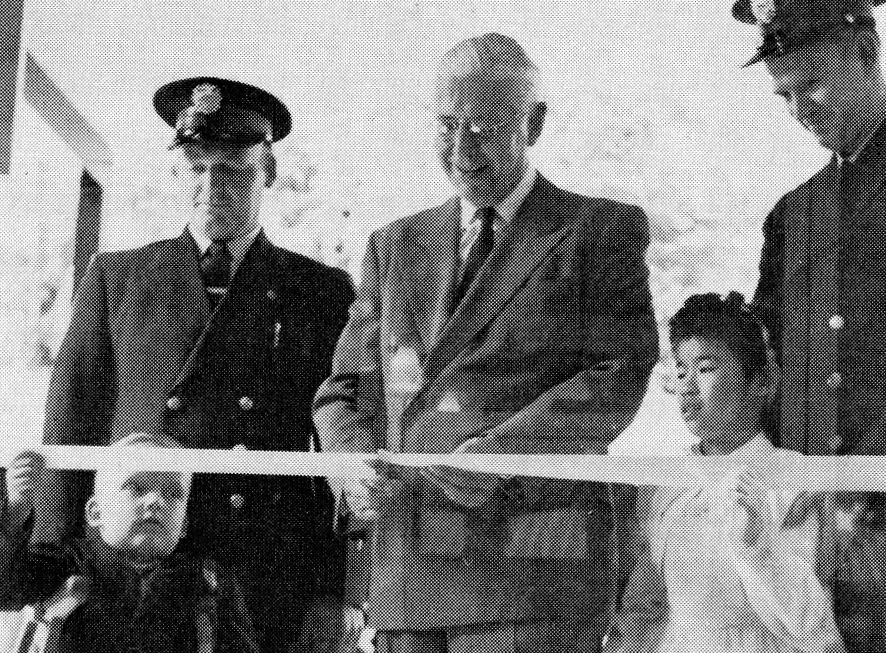
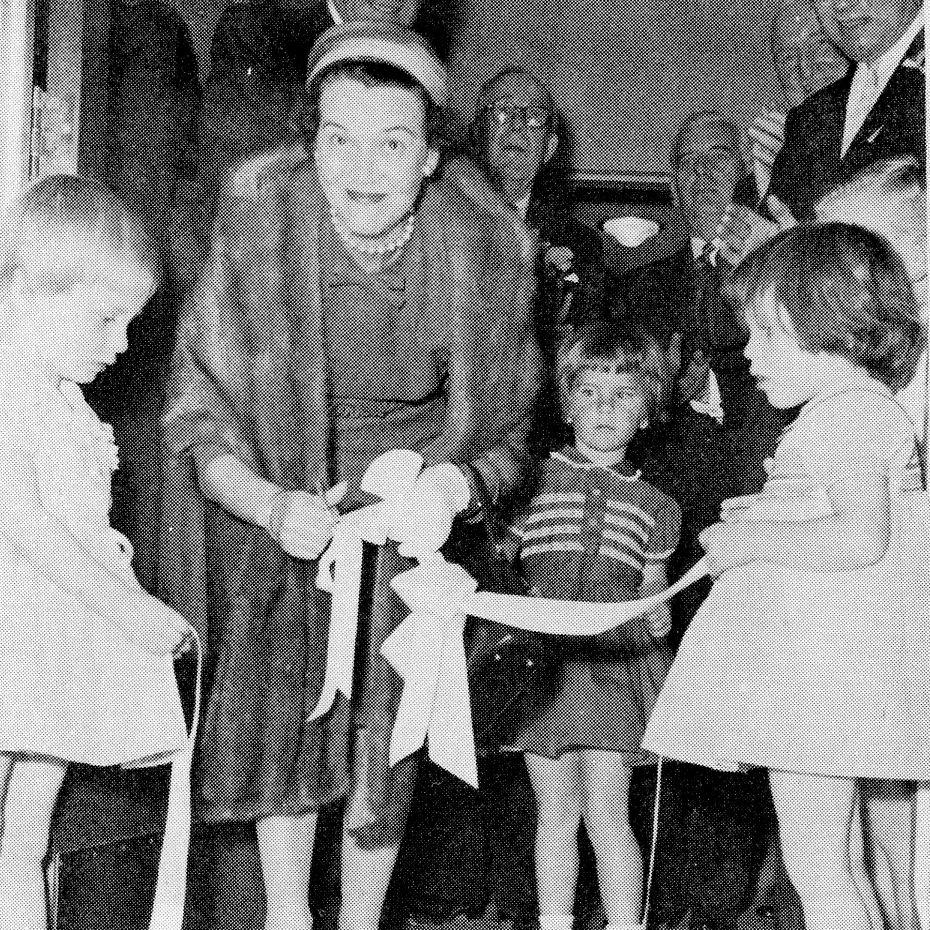
Above: Official Opening of Cancer Clinic’s New Addition
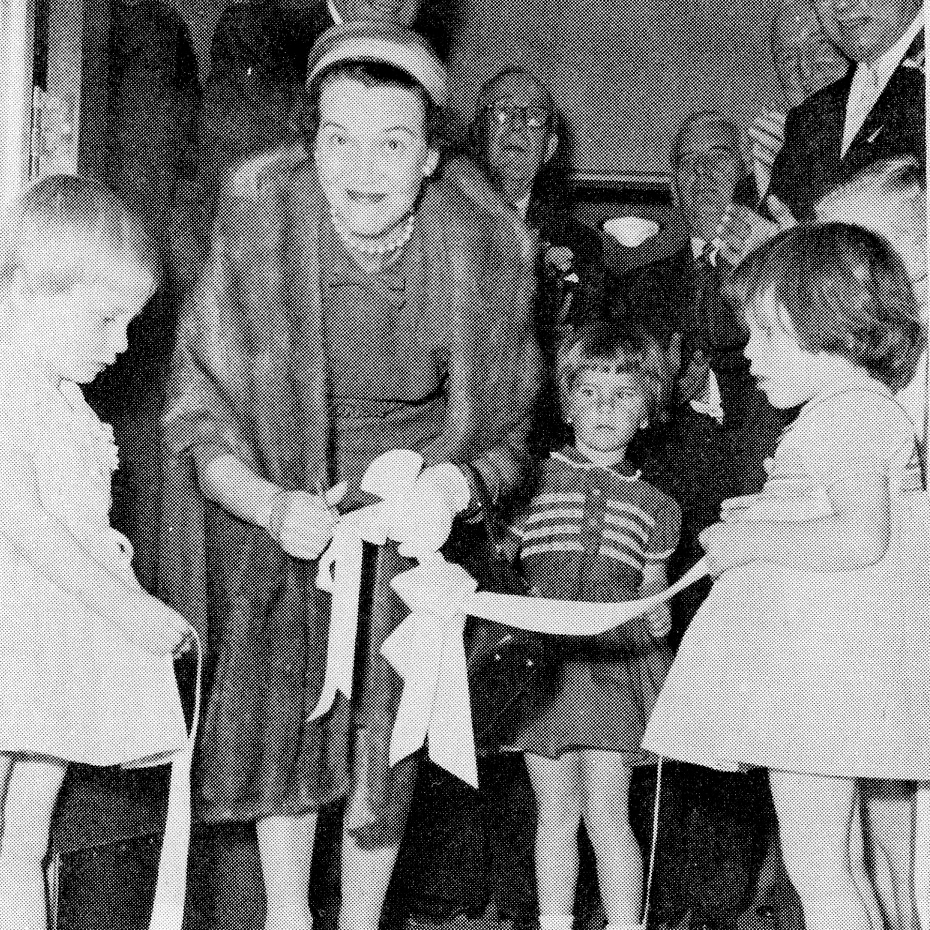
Mrs. Donald Ness cutting the ribbon, assisted by children of Clinic Doctors.
There is an interesting history behind cancer care at LHSC. Now called the Verspeeten Family Cancer Centre, the cancer centre teams through the decades have been leaders in innovation and care delivery. Take a journey through the timeline of cancer care excellence at LHSC.
1932 – The Cody Commission (an Ontario Royal Commission) recommended the establishment of three cancer clinics across Ontario in Toronto, Kingston and London.
1934 – An agreement was reached between the Division of Cancer Control in the Ontario Department of Health and Victoria Hospital to establish a cancer clinic in London.
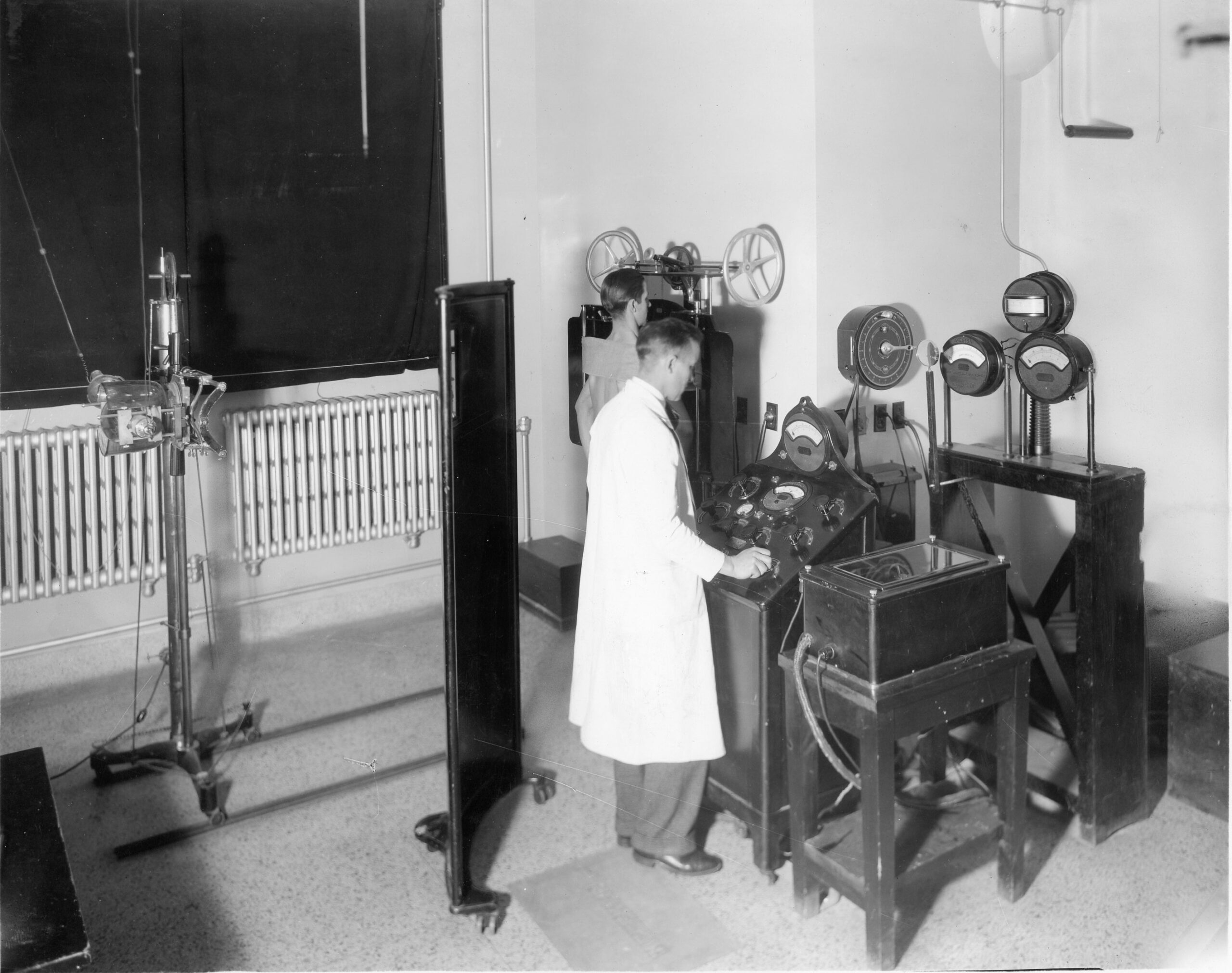
May 26, 1941 – The Ontario Institute of Radiotherapy (OIR) at Victoria Hospital officially opened on South Street.
1943 – Through an act of legislation from the Province of Ontario, the Ontario Cancer Treatment and Research Foundation (OCTRF) was incorporated in 1943. The OCTRF had a mandate to establish and conduct a program of diagnosis, treatment and research for cancer in Ontario, and included assuming the operation of the cancer clinics established across the province.
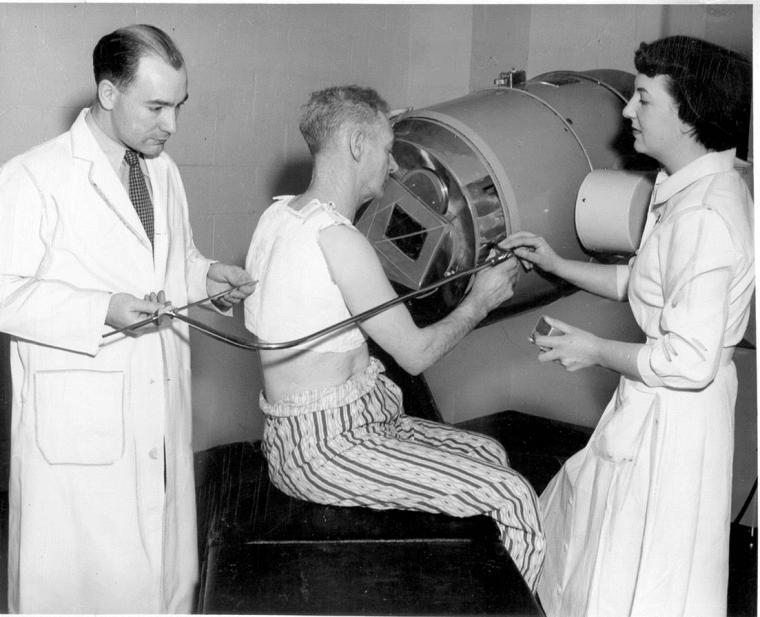
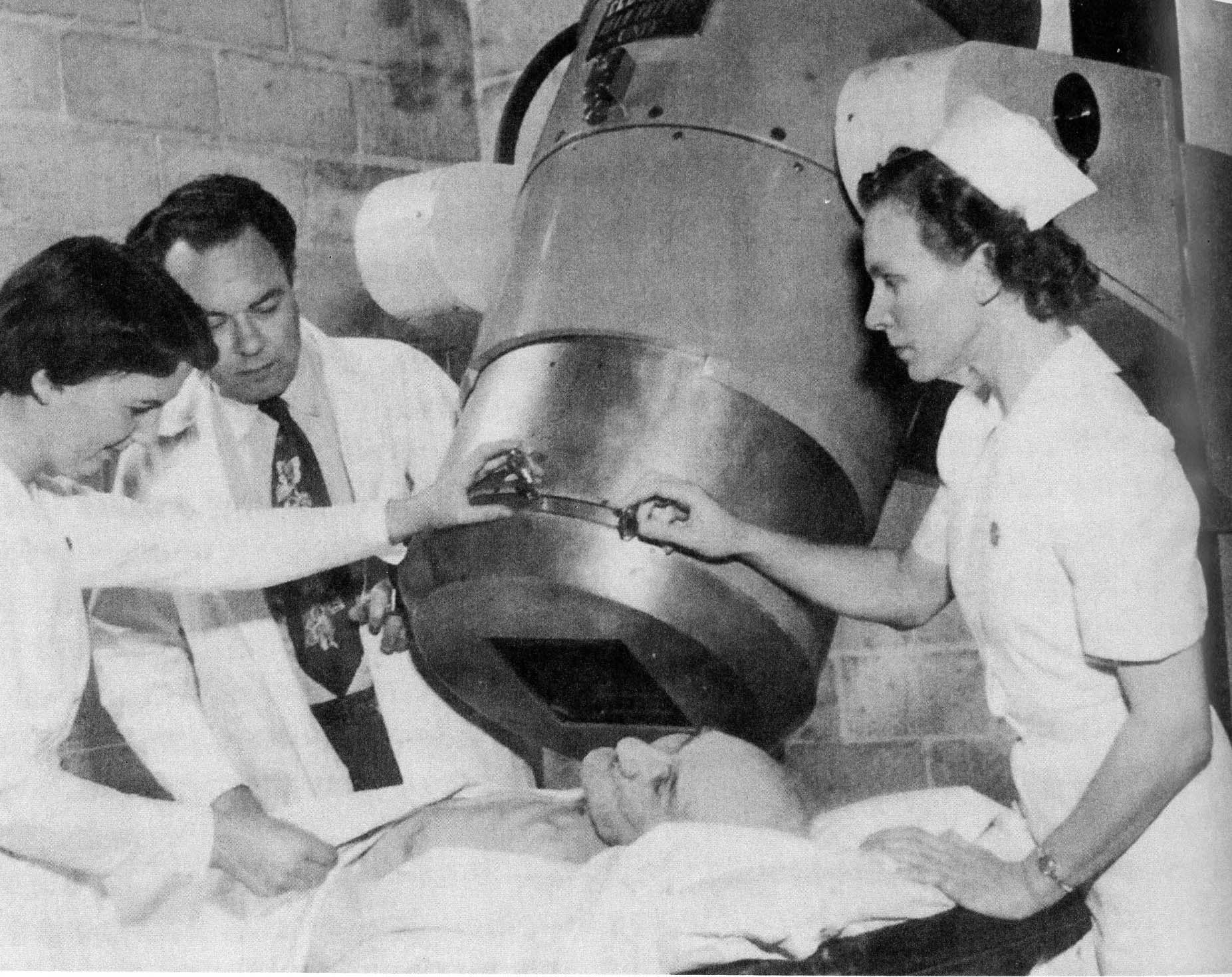
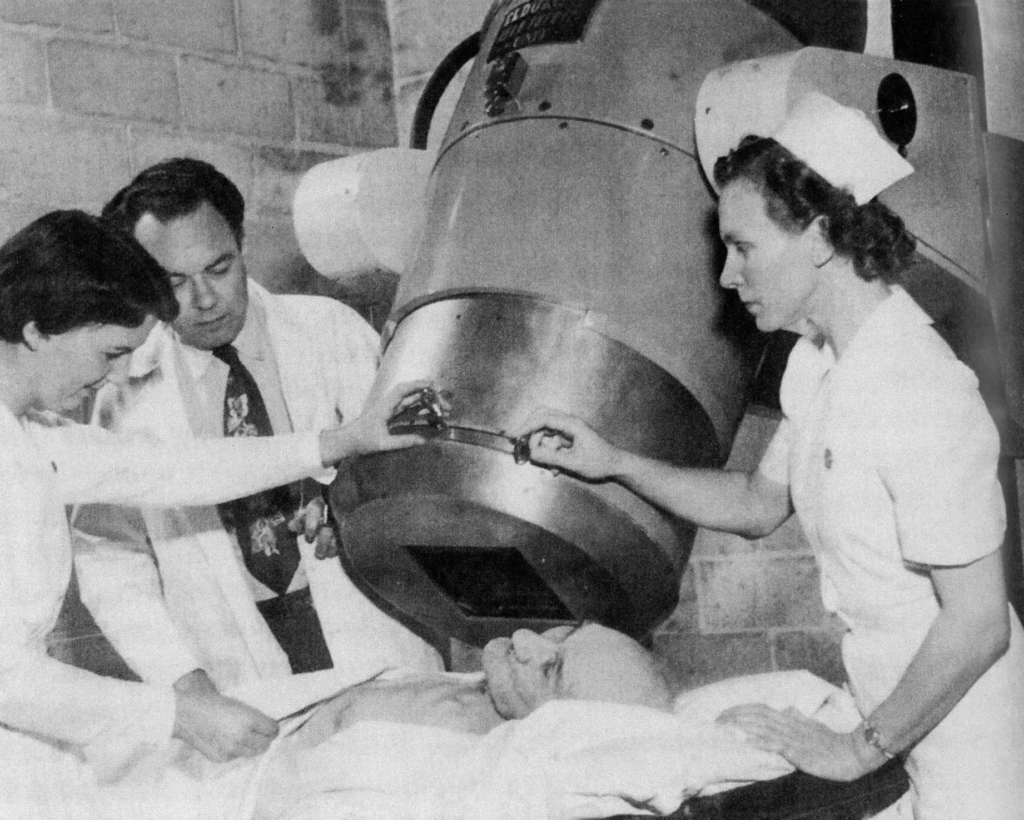
October 27, 1951 – The first treatment in the world with Cobalt-60 radiation took place at the OIR with Dr. Ivan Smith as the attending physician. The machine was known as the “Cobalt Bomb” or “Peace Bomb”, but its formal name was the “Eldorado A.” The machine was developed by Dr. Smith in collaboration with Mr. Roy Errington from Eldorado Mining and Refining Inc. The machine treated 16 new patients per month.
November 18, 1954 – Simultaneously, the OIR became the London clinic of the OCTRF and relocated to a new space. The cancer clinic occupied two floors in the new east wing at Victoria Hospital on South Street. New radiation treatment equipment was added, making it the most modern clinic in Ontario.
1955 – The original Cobalt radiation source was replaced. Also in 1955, the first radioactive isotope laboratory was established and the first researcher, a radiobiologist, joined the London Clinic team.
April 10, 1958 – An addition to the cancer clinic was completed in 1958, and on this date, Dr. J.T. Phair, Consultant to the Ontario Department of Health, officially opened the new addition. The two-storey extension housed the isotope, radiobiology and recreation therapy divisions, and the Junior Cobalt 60 Treatment Room. The opening of the clinic addition is a major health event in the city and surrounding area, providing additional evidence of why London has come to be recognized as one of the outstanding health centres of Canada.

1966 – A new radiobiological research laboratory was added to the cancer clinic.
January 2, 1962 – The first cancer patient was welcomed at the newly opened Thameswood Lodge, which provided accommodation for patients in the region coming to London for treatment.
1970s – Changes continued in the cancer clinic as it grew and as early treatment machines were replaced with modern technology. For example, chemotherapy was introduced as a treatment modality and a chemotherapy suite was added to the cancer clinic. Originally, the suite had two treatment chairs.
1975 – Temporary quarters were built to provide new professional library and research laboratory spaces, primarily for tissue culture research. At this time, the first cancer researcher was appointed.
1984 – The name of the clinic was changed to the London Regional Cancer Centre (LRCC) to reflect an increase in patient activity from outside of London across the southwestern Ontario region. By this time, the LRCC was becoming cramped as operations grew.
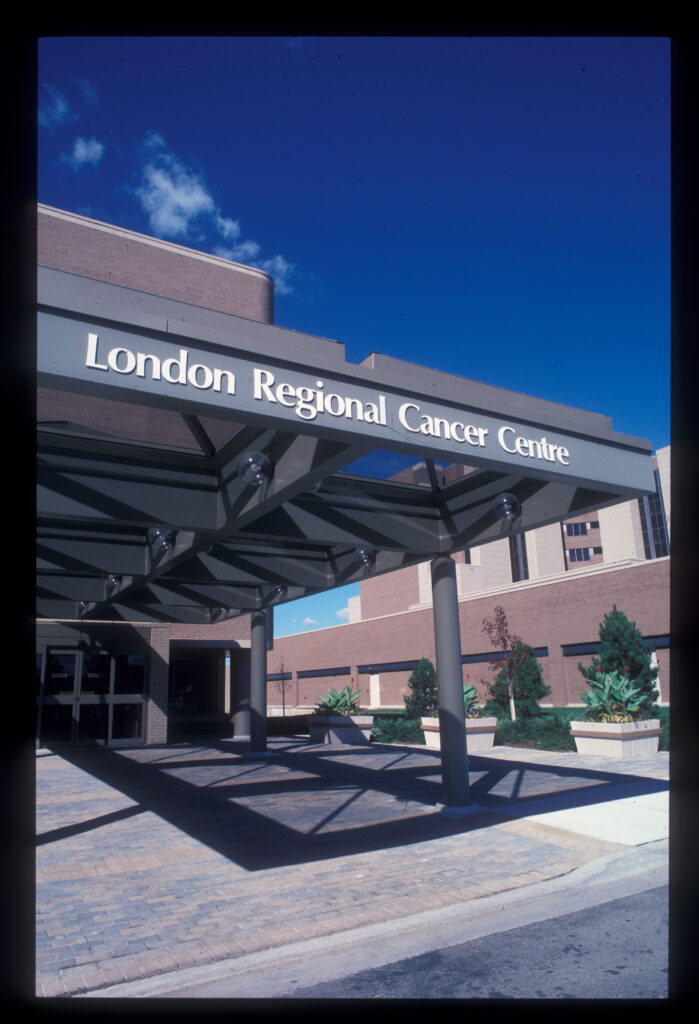
August 1985 – The Ministry of Health approved the construction of a new regional cancer centre on the Westminster site of Victoria Hospital.
May 13, 1988 – The LRCC moved into its new state-of-the-art facility that housed the latest in treatment equipment and had more space for its growing research operations.
The new centre with its open atrium space also focused on providing a sense of well-being for patients and families by including artwork by various London artists throughout the waiting and treatment areas. Local musicians added their unique performances in the atrium at various times to provide a comforting, welcoming and dynamic experience for patients and visitors.
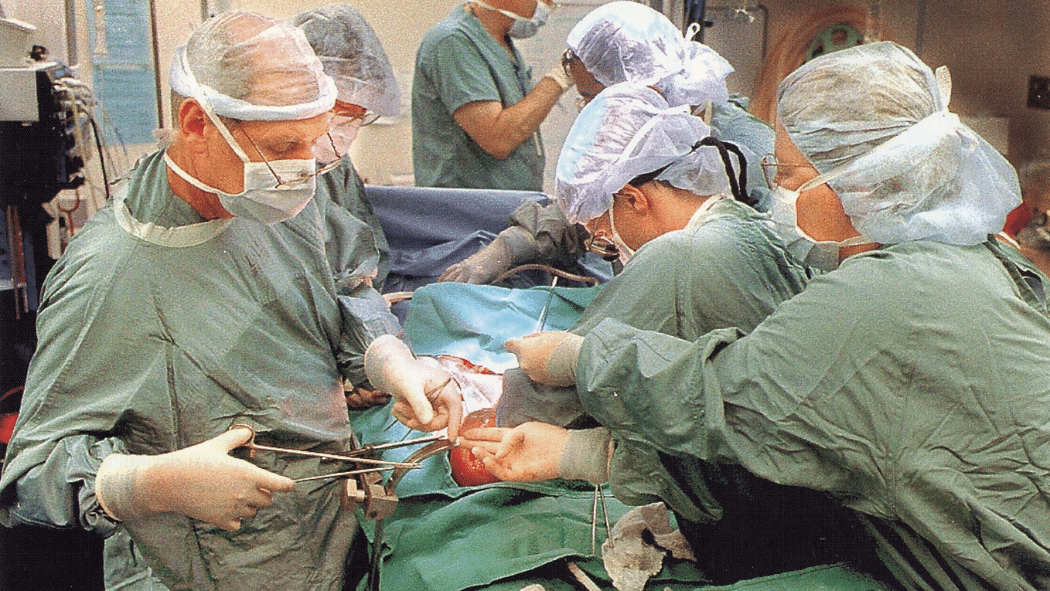
1989 – LHSC performs its first bone marrow transplant to treat a patient with leukemia.
1990 – The cancer centre started using SRS (stereotactic radiosurgery) using a stereotactic frame. This immobilization system allowed radiation oncologists to better aim the radiation at small lesions in the brain, reducing toxicity and cognitive decline compared to conventional treatments at the time.

April 1995 – The OCTRF became Cancer Care Ontario (CCO) and CCO Regional was established to more accurately reflect the growing regional focus of cancer care in Ontario. Southwestern Ontario became the regional component of LRCC. Since then, the Regional Cancer Program has continued to grow and evolve. Community chemotherapy clinics were now available across the region, allowing patients to have access to the care they need closer to their home community and a regional accountability agreement was signed by cancer care providers to forge the Regional Cancer Services Alliance.
1996 – LHSC performs its first stem cell transplant to treat blood cancer using cells collected from a related donor. Donor transplants can reduce risk of relapse or recurrence for some blood cancers like acute leukemia, compared to transplants with self-donated marrow.
1998 and 2004 – Major expansion projects increased treatment capacity in both radiation therapy and chemotherapy and added additional research space.
Late 1990s/Early 2000s: LHSC is one of the first centres in Canada to provide In-111 Octreotide and I-131 MIBG (MIGB is a radioactive substance that helps treat certain kinds of tumours) as part of a collaborative multidisciplinary Neuroendocrine Tumour (NET) Team.
July 2001 – The last Cobalt radiation treatment unit at LRCC was removed. It was replaced by a Tomotherapy unit – the more modern treatment technology. At that time, LRCC was one of only two cancer treatment centres in Canada to have this new technology. The unit had the capability to plan and provide treatment at the same time, treating in slices that are designed to “hit the tumour” and spare the surrounding healthy tissue.
November 2002 – The Ministry of Health and Long-Term Care announced that Cancer Care Ontario would transfer responsibility for direct management and delivery of patient care services to the hospitals as Integrated Cancer Programs.
2003 – The cancer centre started using fractionated stereotactic radiotherapy using a less invasive infrared biteblock system. This new method allowed for a more comfortable, but still effective, treatment for patients with small brain lesions.
January 1, 2004 – The LRCC became the London Regional Cancer Program (LRCP) at London Health Sciences Centre.
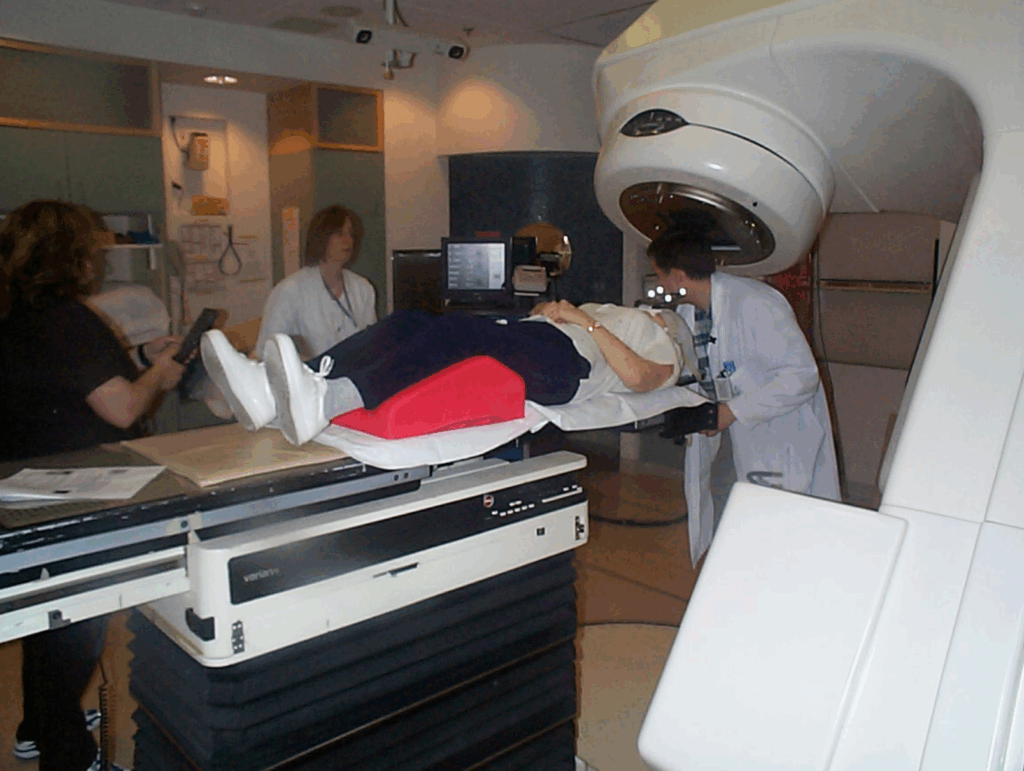
2004 – Clinical implementation of helical tomotherapy: London was chosen as one of two sites in Canada to implement this state-of-the-art image-guided radiation therapy machine. The London team, including physicists and radiation oncologists, collaborated with Rock Mackie, the inventor of tomotherapy, on its initial concepts through to its initial implementation. To date, more than 4,000 patients have been treated with tomotherapy at the Verspeeten Family Cancer Centre.
2004 – Clinical implementation of respiratory gating, including Canada’s first respiratory gated treatments of a liver SABR (stereotactic ablative radiotherapy) patient and lung cancer patient. This technology allowed for treatments to better target radiation to tumours in the thorax and abdomen that are affected by respiratory motion. This technology consists of an infrared camera system that tracks a weightless infrared reflector block. It is placed on the patient and will trigger the radiation beam on only when the patient is at the end of their exhale position. This ensures that less radiation is treated to other healthy organs. More than 1,000 patients have been treated with this technology.
2010 – LHSC is one of the first centres in Canada to provide Lu-177 Dotatate (a receptor targeted radiotherapy) as a treatment option for patients with neuroendocrine tumours.
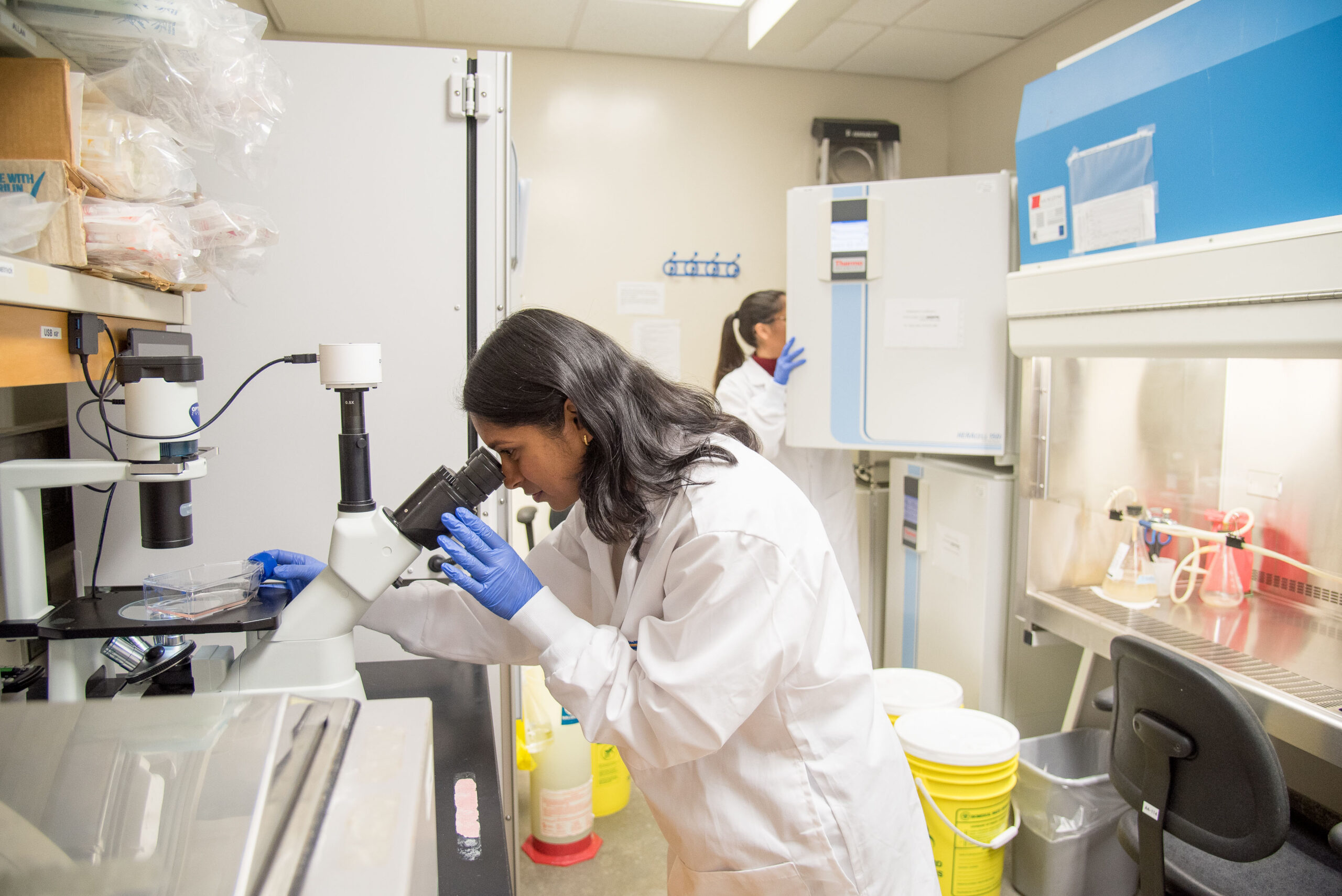
2010 – With a donation of $1 million from the Baines Foundation, along with the support from other community members, the Gerald C. Baines Centre for Translational Cancer Research opened. The Baines Centre facilitates knowledge transfer between teams to pursue research related to major treatment goals such as early detection, prevention, novel therapies and technology platforms with potential for patient application. This centre engages and supports translational cancer research by linking researchers across London, Ontario from multiple disciplines with clinicians. The goal is to ensure that cancer patients throughout southwestern Ontario receive the highest quality of care regardless of where they live.
2012 – The first patient ever that was treated in the SABR-COMET randomized clinical trial for adrenal metastasis (metastasis refers to the spread of cancer cells from where they first formed in the body) and treated with respiratory gated radiotherapy happened at LHSC. This landmark clinical trial, led out of LHSC, was the first to randomize patients with oligometastatic disease (one to five metastatic sites) to either stereotactic radiotherapy or standard-of-care palliation (making the symptoms less severe). This trial created a shift in paradigm as it challenged the traditional view that metastatic cancer is uniformly incurable and provided strong support for aggressive local therapy to metastatic sites in selected patients. This trial influenced treatment guidelines and clinical practice worldwide and is now a treatment option in many centres. This trial also inspired many follow-up studies to refine indications and assess benefits in different cancers of higher metastatic burden.
2012 – First use of immune check-point inhibitors at LHSC for standard-of-care cancer treatment. These drugs revolutionized cancer treatment globally by harnessing the body’s own immune system to recognize and destroy cancer cells. Immunotherapies offer new hope when more traditional chemotherapy treatments have failed or are unlikely to succeed.
2018 – The molecular imaging and theranostics research unit was established due to the high demand for diagnostic imaging and radiopharmaceutical therapy trials to establish new cancer therapies and improve imaging for our patients.
2019 – The Baker Centre for Pancreatic Cancer opened after a gift of $1.5 million from Rick and Shelley Baker. The Baker Centre focuses on the advancement of pancreatic cancer treatment and research.
2019 – LHSC began implementation of the surface-guided radiation therapy and HD-MLCs to treat SRS brain patients with open faced masks and SABR (stereotactic ablative radiotherapy) lung patients with a deep inspiration breath hold technique. This technology uses three infrared camera systems that project a red-speckle pattern on the patient that can be used to ensure proper positioning of the patient in real-time. The radiation beam is enabled only when the patient is in the correct position.


2020 – A state-of-the-art, first of its kind facility in Canada – the Verspeeten Clinical Genome Centre – opened at LHSC after a $3 million gift from Archie and Irene Verspeeten. The research centre helps physicians provide more accurate diagnoses, predict the progress of a patient’s disease and provide more targeted treatments – individualizing patient care. The centre’s initial focus was on genomic sequencing for pancreatic cancer alongside the Baker Centre for Pancreatic Cancer.
2020 – The first patient in the world treated on the ARREST clinical trial that established safety and feasibility of SABR (stereotactic ablative radiotherapy) to all sites of polymetastatic disease (more than 10 metastases). This was the first trial in the world of its kind.
2022 – First patient treated on the “ARGOS-CLIMBER” SABR Prostate Clinical Trial that aimed to establish safety and feasibility of treating the prostate with a focal boost guided by multiparametric MRI and 18F-PSMA-1007 PET using SABR. This trial demonstrated acceptable 6-month toxicity using 5 fraction SABR with PET/MRI directed SIB to the prostate and lymph nodes.
2022 – First patient treated on the ANSR-PDAC clinical trial that aims to establish safety and feasibility of treating resectable and borderline-resectable pancreatic cancer patients with SABR in only three fractions and to assess the treatment response. The assessment includes examining changes in blood flow to the area and to the immune system. Pancreatic tumours notoriously have low blood flow due to a rich stroma surrounding them. This trial examines whether SABR can temporarily increase blood flow providing a window of opportunity to provide more effective systemic therapy to pancreatic cancer patients in the future.
November 2023 – The Blood and Marrow Transplant Program (BMTP) at LHSC became accredited by the Foundation for the Accreditation of Cellular Therapy (FACT). This internationally recognized accreditation reflects the highest level of organizational commitment to quality standards in cell collection, processing and clinical care associated with stem cell transplantation.
April 29, 2024 – After a historic $20 million donation from Archie and Irene Verspeeten in 2023, facilitated through the London Health Sciences Foundation, the LRCP is renamed the Verspeeten Family Cancer Centre. The donation is the largest foundation gift ever given in the history of southwestern Ontario and is being used to improve patient care, establish the Verspeeten Chair in Translational Cancer Research, enhance the Verspeeten Clinical Genome Centre, and support Medical Oncology and Radiation Oncology fellowships to attract the next generation of specialists.
October 2024 – A team at London Health Sciences Centre Research Institute (LHSCRI) is the first in Canada to treat a patient with neuroendocrine tumours (NETs) – a rare form of cancer – using a radioisotope (an atom that releases radiation) called actinium-225 DOTATATE. The treatment is a type of therapy called theranostics, which combines advanced diagnostic imaging technologies and radioisotopes to precisely locate tumours and then eradicate them by releasing radioactive energy.
December 27, 2024 – LHSC is the first hospital in Canada to provide publicly-funded Novartis PLUVICTO™ treatment for prostate cancer. The new therapy targets cancerous cells and was researched and trialed globally, including at LHSC. It is now funded through Ontario’s Ministry of Health as a standard treatment option for patients with advanced-stage prostate cancer. LHSC participated in the multinational VISION trial starting June 10, 2019. This trial led to the Pluvicto funding.
2024 – The Verspeeten Family Cancer Centre surpassed 40,000 total visits to the systemic suite in a single year.
Today – The Verspeeten Family Cancer Centre is the cancer services program of LHSC. The Ministry of Health and Long–Term Care provides partial funding to Verspeeten Family Cancer Centre through Cancer Care Ontario.
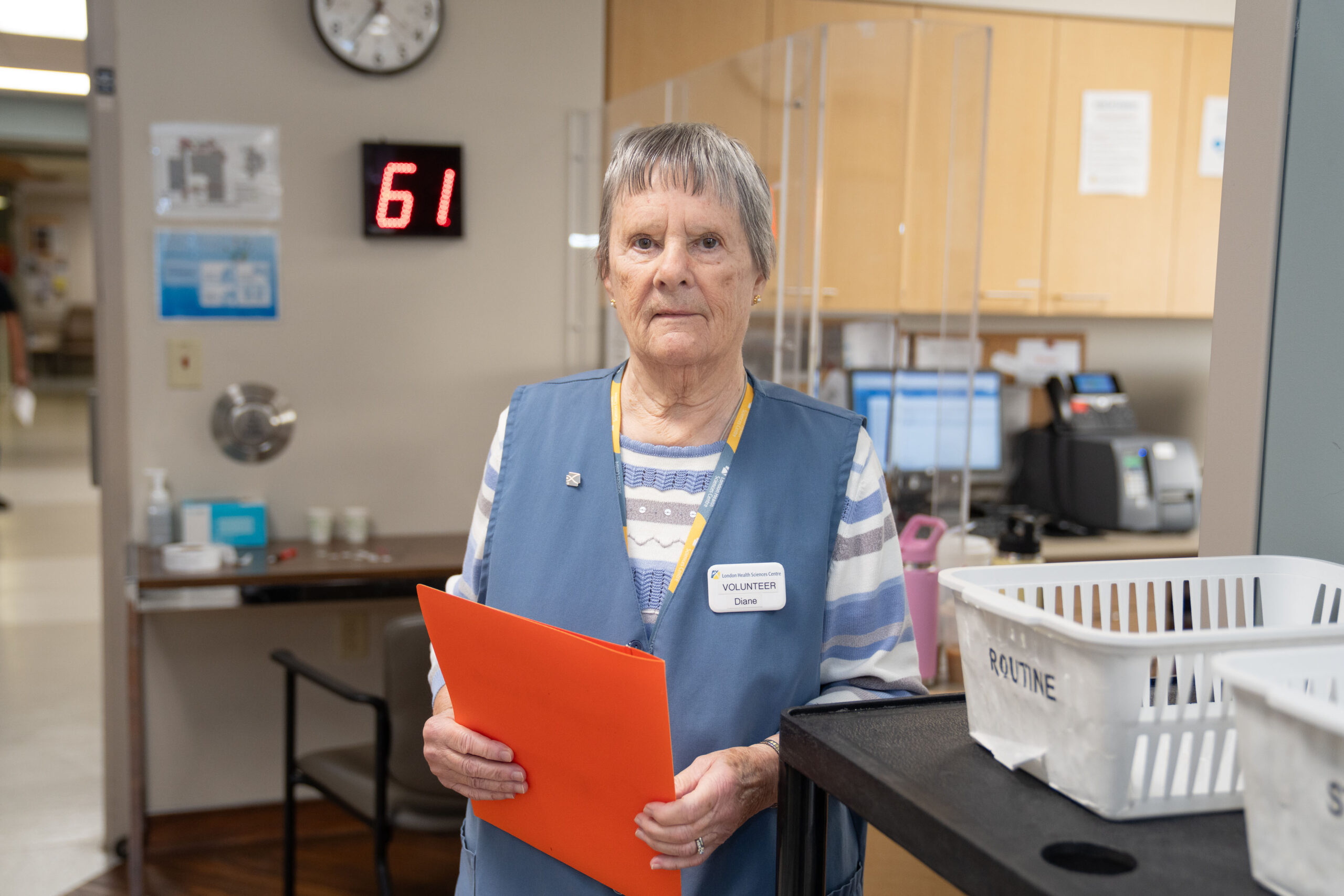
Now, with 25,809 patients seen between April 1, 2024 and March 31, 2025, the Verspeeten Family Cancer Centre provides inpatient and outpatient cancer care including radiation therapy and chemotherapy as well as a full range of support services to help cancer patients and their families throughout the treatment process. As the regional cancer centre, members of the Verspeeten Family Cancer Centre healthcare team work closely with community healthcare professionals in the region to plan and coordinate care for patients across southwestern Ontario.
The cancer research program through London Health Sciences Centre Research Institute (LHSCRI) has experienced significant growth over the decades, providing access to clinical trials to patients across southwestern Ontario. Some of the milestones in treatment options that have become available at the Verspeeten over the past several decades include targeted therapies and immunotherapies, pharmacogenomics and personalized medicine (which uses a patient’s genetics to inform treatment decisions) and stereotactic radiosurgery, among others. Through clinical trials through LHSCRI, the Verspeeten has access to cutting edge therapies that have potential to transform patient care.
The Verspeeten Family Cancer Centre has a long, distinguished history in providing excellent care to the people of London and Southwestern Ontario (with a catchment area including the counties Middlesex/London, Elgin, Oxford, Perth, Huron, Grey, Bruce, and part of Norfolk) and will continue to not only provide world-class care but also fulfill its missions in innovation for education and research into the future.
LHSC is celebrating 150 years of care, innovation, and community impact by sharing 150 moments from our history. Join us in marking this milestone by sharing your own LHSC story.