Meet your surgeon and their robot: The unstoppable duo behind cutting-edge surgeries at LHSC

Above: Dr. Sandrine de Ribaupierre Associate Scientist at LHSCRI and Paediatric Epilepsy Neurosurgeon, demonstrates the ROSA Robotic Arm. Dr. de Ribaupierre, in collaboration with the University Hospital Epilepsy Program at LHSC, including Dr. Jonathan Lau, performed the Canadian First Radiofrequency Thermocoagulation procedure on 11-year-old Makayla Douglass
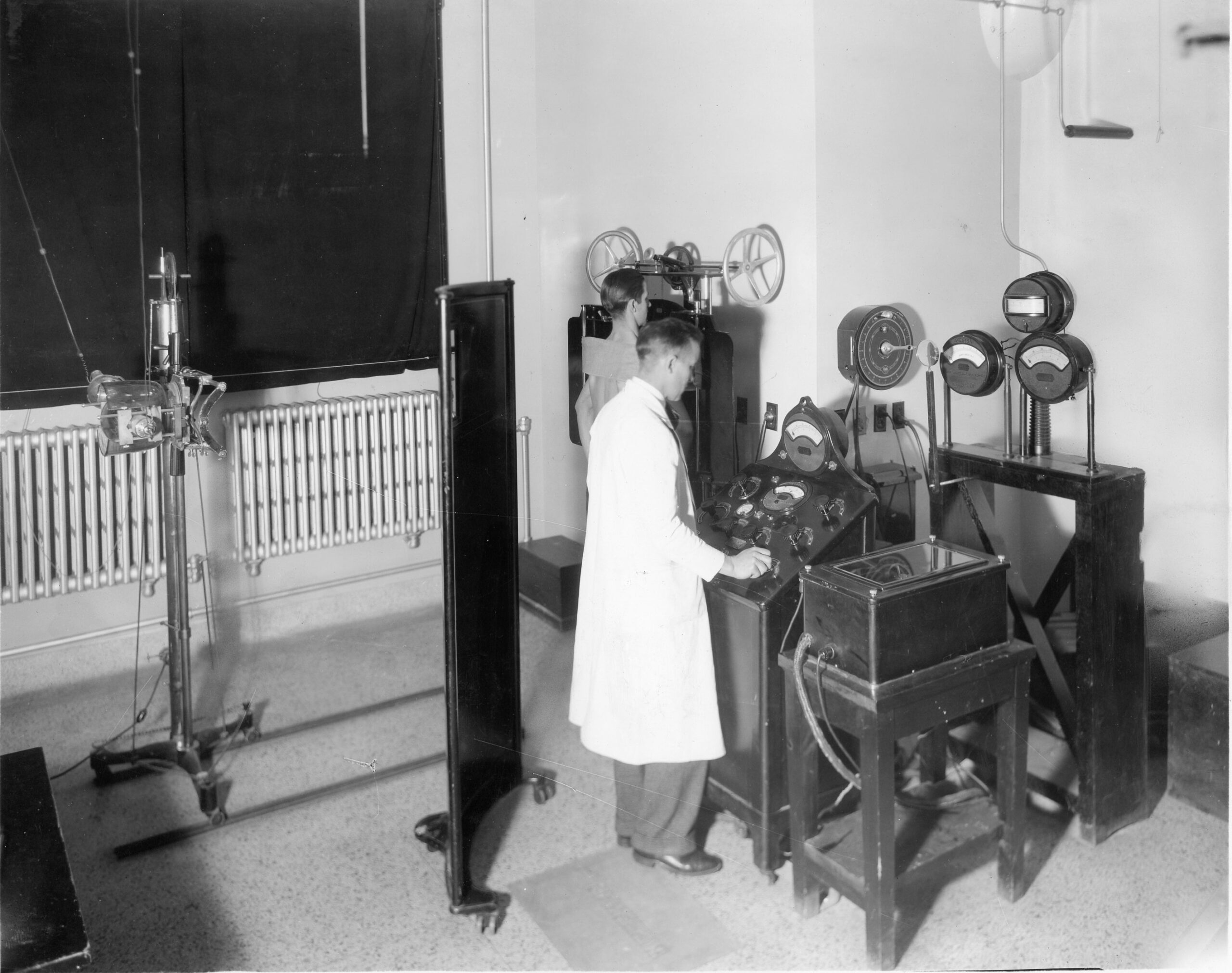
Since the early 2000s, major breakthroughs in surgical robotics have redefined what is possible and have advanced patient care, innovation and research.
At the forefront of robotic-assisted surgeries is London Health Sciences Centre (LHSC). As LHSC celebrates 150 remarkable years, robotic research in the early 2000s comes to mind for many who have pioneered surgical procedures and enhanced the standard of care for patients worldwide.
A world-first milestone in robotic-assisted surgery
The approaching turn of the century brought fears of Y2K, a computer bug that many believed would cause widespread failures. However, cutting-edge technological advancements in health care did not slow down at LHSC. Instead, they advanced.
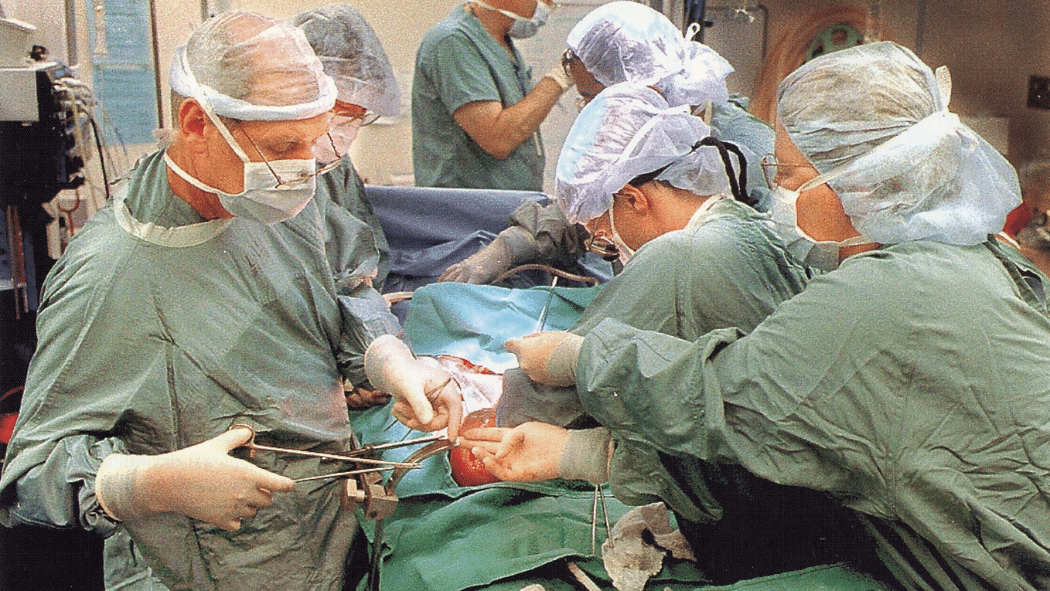
One of the biggest milestones leading up to the year 2000 was the world’s first closed-chest, robotic-assisted coronary bypass surgery completed by Drs. Douglas Boyd and Reiza Rayman at LHSC’s University Hospital. The procedure helps create a new path for blood to flow around blocked heart arteries.
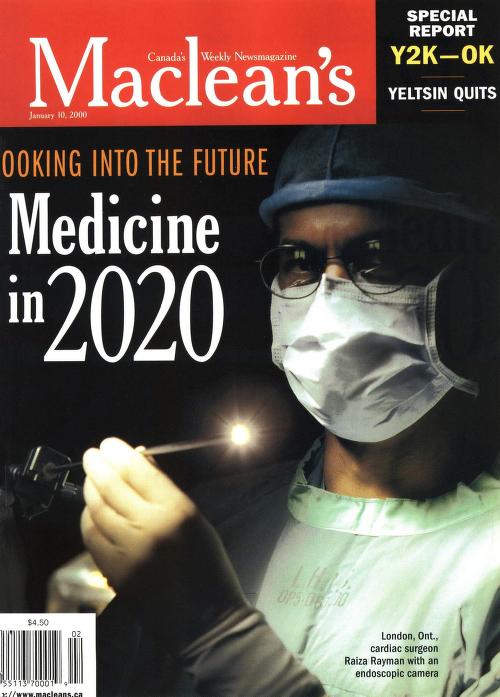
Capturing the attention of outlets like Maclean’s, Dr. Doug Boyd and his team conducted the surgery using one of the most advanced medical robots of its time, the NASA-designed ZEUS. Unlike traditional open-heart surgery at the time, which involved a large incision and stopping the heart, the surgeons used a console to guide ZEUS in operating on a beating heart through small incisions. The ZEUS robot gave the surgeons incredible control and steadiness, allowing them to stitch tiny heart blood vessels with extreme accuracy – even smaller than a millimeter.
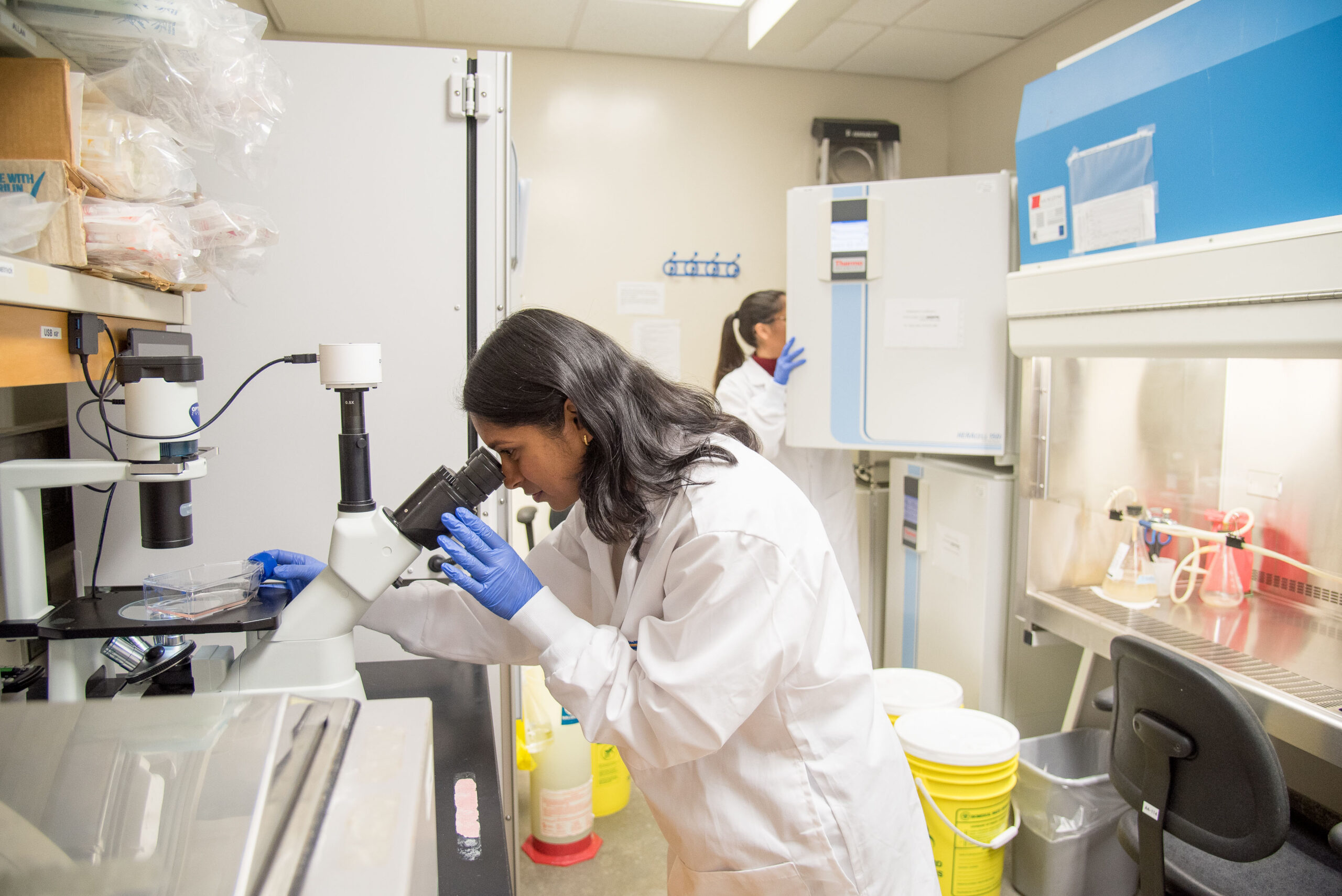
A world-renowned surgical centre for training, education and research
The pioneering spirit of researchers who sought to learn more in robotic-assisted surgeries contributed to the opening of the world-leading Canadian Surgical Technologies and Advanced Robotics (CSTAR) at LHSC’s University Hospital and the recruitment of Dr. Christopher Schlachta, Scientist at London Health Sciences Centre Research Institute (LHSCRI) and Medical Director of Surgery at University Hospital. Inside this state-of-the-art space is where some of the most exciting work in robotic-assisted surgery and medical training is happening.
Spanning 22,500 square feet, CSTAR brings together researchers, engineers, educators and clinicians to test new surgical robots, practice surgeries in high-tech simulations rooms, and develop life-saving techniques. As an accredited simulation centre of the American College of Surgeons and the Royal College of Physicians and Surgeons of Canada, CSTAR also trains the next generation of health-care providers not only those at LHSC, but also those from around the world.
From the day CSTAR opened its doors to today, the brightest minds train, educate and research new ways of making surgeries safer, faster, and smarter. And for the trainees, engineers, clinicians and researchers who walk its halls, it’s a place where ideas turn into real-world breakthroughs that improve outcomes for patients.
The art of precision: LHSC welcomes the da Vinci surgical robot
In 1999, LHSC acquired the da Vinci Surgical System to conduct procedures for a variety of health conditions in minimally invasive ways. Today, LHSC has purchased one of the latest da Vinci Surgical Systems, which not only is able to assist in minimally invasive surgeries but also powered by the latest innovations of modern-day science and technology, including artificial intelligence.
Controlled by an LHSC surgeon at a console, this robotic system performs operations through tiny incisions with more precise movements than the human hand alone could manage. Its name is no coincidence. It pays tribute to Leonardo da Vinci, the Renaissance genius who seamlessly merged art, science, and anatomy. Centuries before robotic surgery existed, Leonardo sketched some of the most detailed anatomical drawings in history and envisioned machines that mimicked human movement. Today that vision is alive and its impact is felt at LHSC.
Surgeons expand robotic-assisted surgery research
From the time of the first robotic-assisted coronary bypass surgery to today, the potential of robotic-assisted procedures continues to grow and transform care for a growing number of health conditions.
Orthopaedic surgeries
At LHSC’s University Hospital, joint-replacement surgeries are common. As a hub for robotic orthopaedic research initiatives, surgeons have been at the forefront of innovation. Most recently, LHSC became the first hospital in Canada and one of only half a dozen institutions in the world to have all four major hip and knee replacement surgical robots on site.

“Having all four robots means patients have access to the latest technology and the best possible results,” says Dr. Brent Lanting, Associate Scientist at LHSCRI and Orthopaedic Surgeon at LHSC. “Prior to robotic assistance, patients would get the same alignment of their joint replacement. Today, we can personalize their surgery by getting real-time anatomic and biomechanical assessments of a patient during procedures, enabling surgical decision making and personalized implant positioning.”
Neurological surgeries
Robots are also tested, researched and used for neurological conditions, like epilepsy.
In June 2023, LHSC surgeons became the first in Canada to use a robot called the Renishaw neuromate® to assist in deep brain stimulation surgery, treating seizures caused by epilepsy. The procedure involves placing electrodes in the brain that are connected to a pacemaker, which provides stimulation to alter brain activity enough to prevent or limit seizures.

“Seizures have a substantial negative impact on quality of life,” says Dr. Jonathan Lau, Associate Scientist at LHSCRI and Neurosurgeon at LHSC. “Robotic assistance helps to increase both the accuracy and efficiency of the interventions we can offer, which means many patients – both adults and children – can get back to what they most enjoy doing in life. We have to date performed over 250 robot-assisted procedures for epilepsy.”
Just two years ago, Children’s Hospital at LHSC received the ROSA One Brain, a state-of-the-art robotic arm which assists in surgery to treat epilepsy. One of the first patients to receive treatment using ROSA with Dr. Sandrine de Ribaupierre, Associate Scientist at LHSCRI and Paediatric Epilepsy Neurosurgeon, was 11-year-old Makayla Douglass who experienced seizures as a result of epilepsy since she was one year old. At worst, Makayla would experience multiple seizures an hour at night.
Makayla’s parents agreed to the minimally invasive procedure which was a success and reduced Makayla’s seizures by 70 per cent the first time. Because it was so successful, the family opted to have the same procedure done a second time, which resulted in Makayla being seizure free.
Spinal surgeries
Research techniques and robotic-assisted surgeries are growing at a record pace at LHSC. Dr. Victor Yang, Scientist at LHSCRI, a surgeon at LHSC, and an engineer, is part of that growth and development leading robotic-assisted surgeries for patients with back pain and mobility issues.
In early 2024, Dr. Yang performed Canada’s first robot-assisted direct lateral spine surgery using the Mazor X Spinal Robot at LHSC for debilitating sciatica pain, which occurs when a nerve in the back called the sciatic nerve is compressed or irritated.
“LHSC is the first institute in Canada with two Mazor spinal robots, one on each campus, to serve our local community,” says Dr. Yang. “We continue to research on different techniques in robotic-assisted spinal surgeries and hopefully more patients will benefit from these cutting-edge devices.”
The procedure easily combined what would traditionally require two separate surgeries into a single minimally invasive operation, resulting in reduced surgical time, faster recovery, and relief from debilitating sciatica back pain.
Thoracic surgeries
Thoracic surgery focuses on the treatment of diseases in the chest and has undergone a major transformation with the integration of surgical robotics and advanced research. At the forefront of this field is Dr. Richard Malthaner, researcher at LHSCRI and Chair of Thoracic Surgery at LHSC.
As early as 2001, Dr. Malthaner made history by performing the first robotic-assisted lung volume reduction surgery in the world. The operation was done to help patients with severe emphysema, a lung disease that damages air sacs and makes breathing very difficult, even during simple activities like walking. In this condition, parts of the lung become over inflated and stop working well, which puts extra strain on the rest of the lungs. By carefully removing the most damaged areas using robotic technology, Dr. Malthaner helped patients breathe more easily and set an important example for how advanced surgery could improve lives.
In 2004, Dr. Malthaner made history by performing the world’s first lung cancer surgery that combined a surgical robot with a 3D ultrasound probe. This innovative approach allowed him to remove a cancerous spot from a patient’s lung with remarkable precision. The ultrasound provided real-time images inside the chest, guiding the robot’s movements and reducing the need for large incisions. This breakthrough marked a major step forward in minimally invasive surgery and set the stage for future advances in robotic-assisted procedures.
Building on his world-first achievements, Dr. Malthaner has also pioneered robotic surgery in Canada. He performed the country’s first robotic-assisted esophagectomies to remove cancerous esophagus tissue, the first emergency Nissen fundoplication to repair a dangerous stomach hernia, the first resection of a pericardial cyst, a rare sac near the heart, and the first lobectomy to remove a cancerous spot on a lung, bringing advanced robotic research and care to patients nationwide.
Gastrointestinal surgeries
LHSC surgeons have a longstanding track record of leading the country in the application and evaluation of robotic surgery to gastrointestinal conditions including colorectal, hepatobiliary, gastric bypass, and transplantation, with several world and Canadian firsts along the way.
In 2008, Drs. Andreana Bütter, Associate Scientist at LHSCRI and Paediatric Surgeon at Children’s Hospital at LHSC, and Christopher Schlachta performed the world’s first, entirely robotic intestinal bypass for superior mesenteric artery syndrome – a surgery that helps food go around a blocked part of the small intestine so it can pass through more easily. Surgeons used one of the most cutting-edge surgical robots, the da Vinci. This allowed a 16-year-old high school student to return to classes weeks earlier than other surgical options at the time.
“The remarkable dexterity of da Vinci technology, along with 3D visualization, allows the surgeon to get necessary details about their patient while avoiding the need for larger, painful and unnecessary incisions,” says Schlachta.
Urologic surgeries
The urology team at LHSC has pioneered the use of state-of-the-art robotic technologies in urological care, particularly using the da Vinci Surgical System to enhance precision and minimize patient recovery times. Since performing Canada’s first robot-assisted prostate surgery in 2004, the urology team at LHSC has remained a leader in using advanced, less invasive techniques to treat both cancerous and non-cancerous urological conditions in Canada and around the world. Their expertise, from removing part or all of the kidney to treat cancer, to Canada’s first single port living donor nephrectomy, a surgical procedure to remove all or part of a kidney, and now to robot-assisted bladder cancer removal surgery attracts numerous learners from across the globe.
“The focus of our research on optimizing surgical outcomes by improving how tumours are located, reducing blood loss, and enabling faster recovery with fewer complications has led to immediate patient benefits, including shorter hospital stays, less pain, and quicker returns to normal activities”, says Dr. Alp Sener, Scientist at LHSCRI Division Head of Urology at LHSC, and the Keith and Leanne Lavergne Chair of Urology at the Schulich School of Medicine & Dentistry and LHSC. “The integration of robotics into urology not only marks a significant advancement in patient care but also contributes to global knowledge in the field.”
Gynecological surgeries
The gynecological team at LHSC is one of the earliest adopters and performs one of the highest volumes of robotic-assisted surgeries in the hospital. Their experience with robotic technology dates back to 2012 when LHSC acquired the first da Vinci robot, allowing surgeons, nurses, and research staff to receive hands-on training in the latest robotic techniques.
Today, robotic assistance is used for a variety of gynecological procedures, including hysterectomies (removal of the uterus due to conditions such as endometrial cancer and pre-cancer, abnormal bleeding, or pelvic pain), and pelvic floor repairs which are needed for conditions like prolapse which can develop because of pelvic muscle weakness.
The addition of the robot has proven to be invaluable in allowing for the ability to provide minimally invasive procedures to patients that would otherwise not be suitable candidates for this type of surgery. Primarily Patients with a high body-mass index (BMI) who would otherwise require much more invasive approaches that result in greater risk of complications both in the operating room and during the recovery phase. By using robotic tools that allow for smaller incisions, greater precision, and enhanced visualization during surgery, the gynecology team at LHSC has helped patients experience less pain, shorter hospital stays, and faster recoveries.
The future of robot-assisted surgery is limitless
Robotic-assisted surgery offers patients precision, safety and efficiency, all while being led by skilled surgeons. At LHSC, clinicians, researchers, and engineers are unstoppable in their pursuit of safer surgeries, faster recoveries, and even cures for debilitating health conditions. From sewing an artery on a beating heart through a tiny incision to performing delicate spinal procedures where a single millimeter can mean the difference between paralysis and recovery, robotic-assisted surgeries and the LHSC innovators behind them are redefining what’s possible in medicine.
LHSC is celebrating 150 years of care, innovation, and community impact by sharing 150 moments from our history. Join us in marking this milestone by sharing your own LHSC story.