From the UH 50 Archives: Cardiac Care at heart of University Hospital

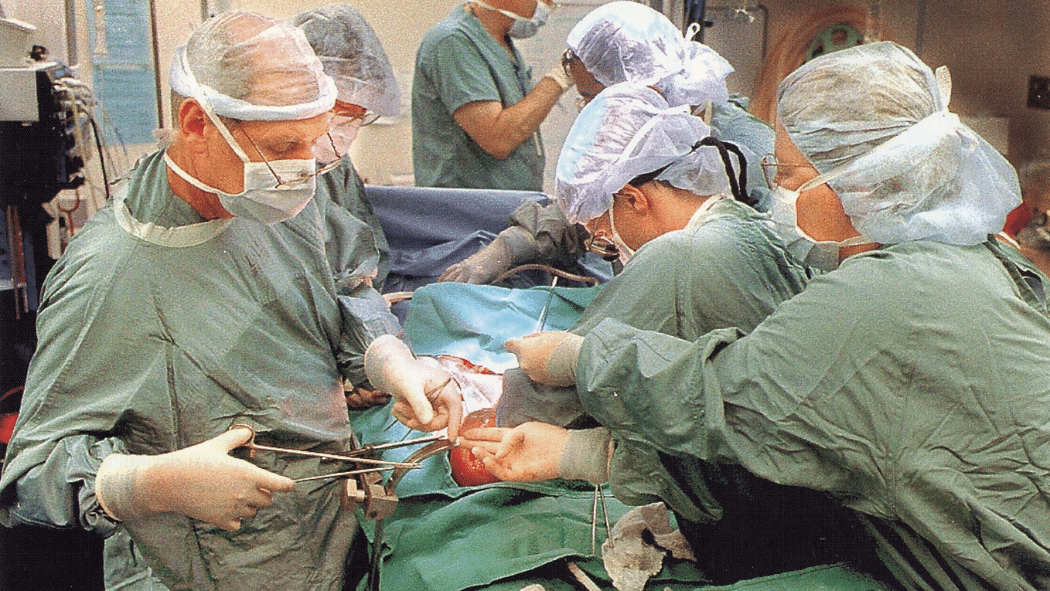
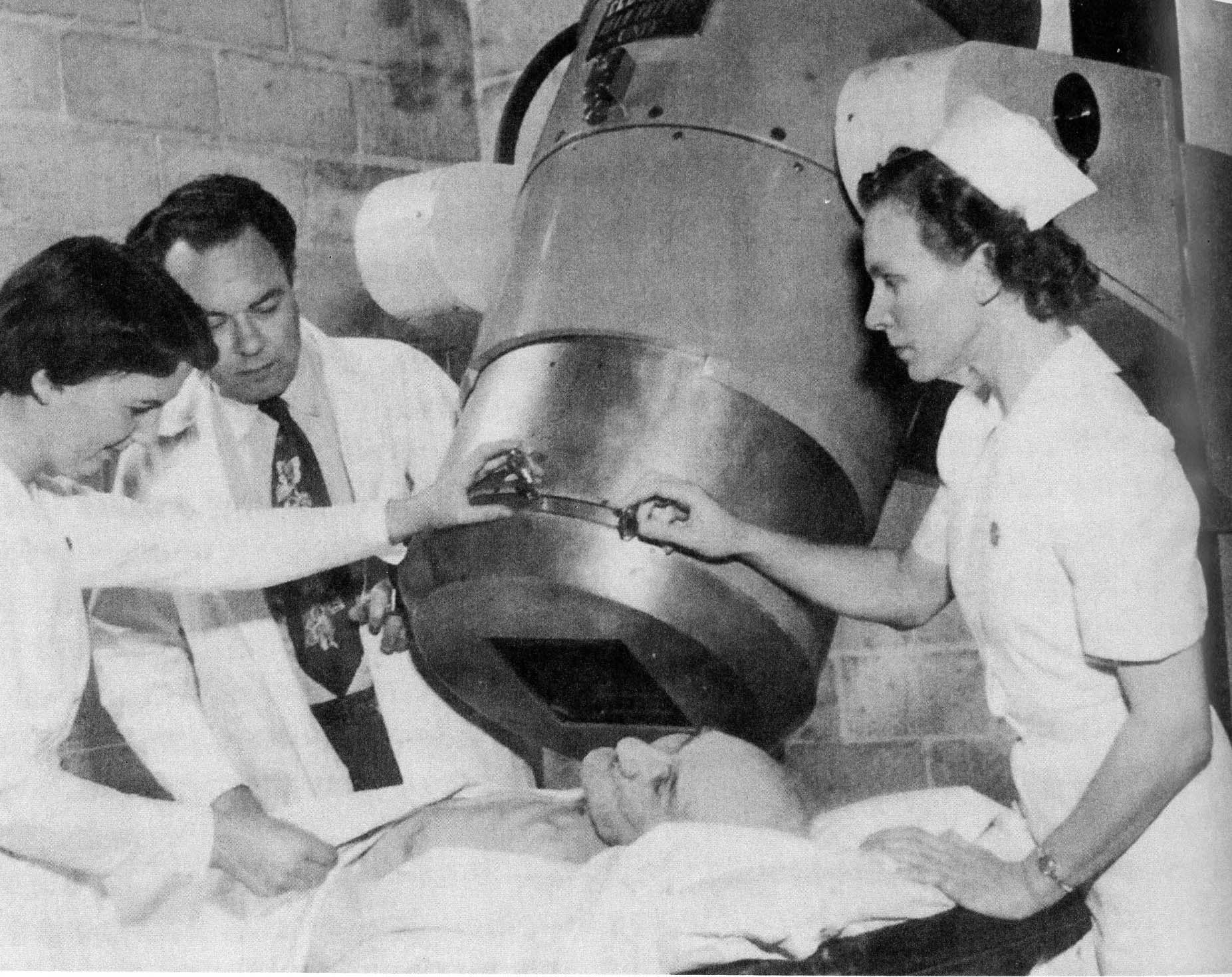
Above: The late Dr. Neil McKenzie and his team perform surgery in the 1980s.
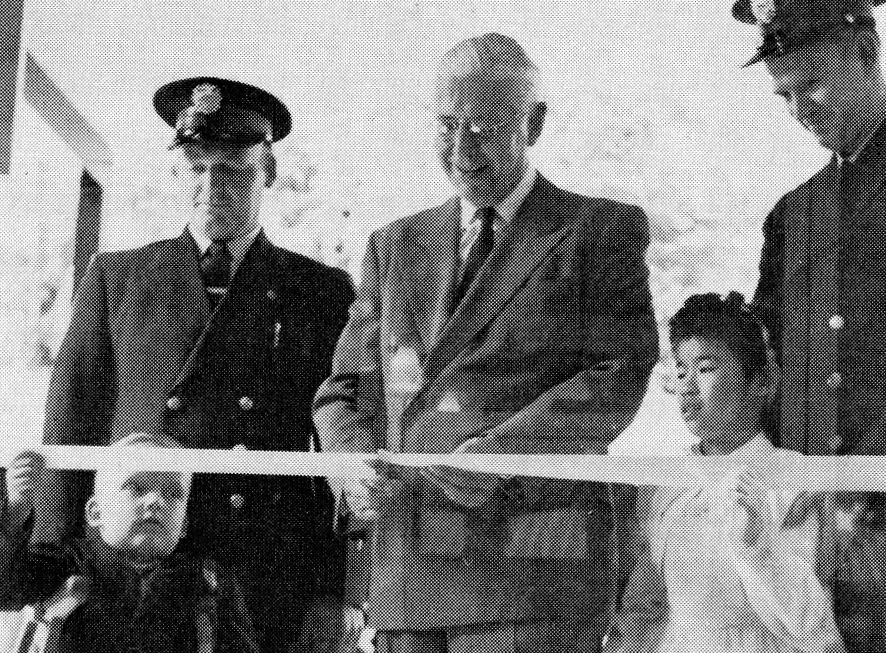
The developments in cardiovascular medicine over the years following the opening of London Health Sciences Centre’s University Hospital (UH) in 1972 were staggering.
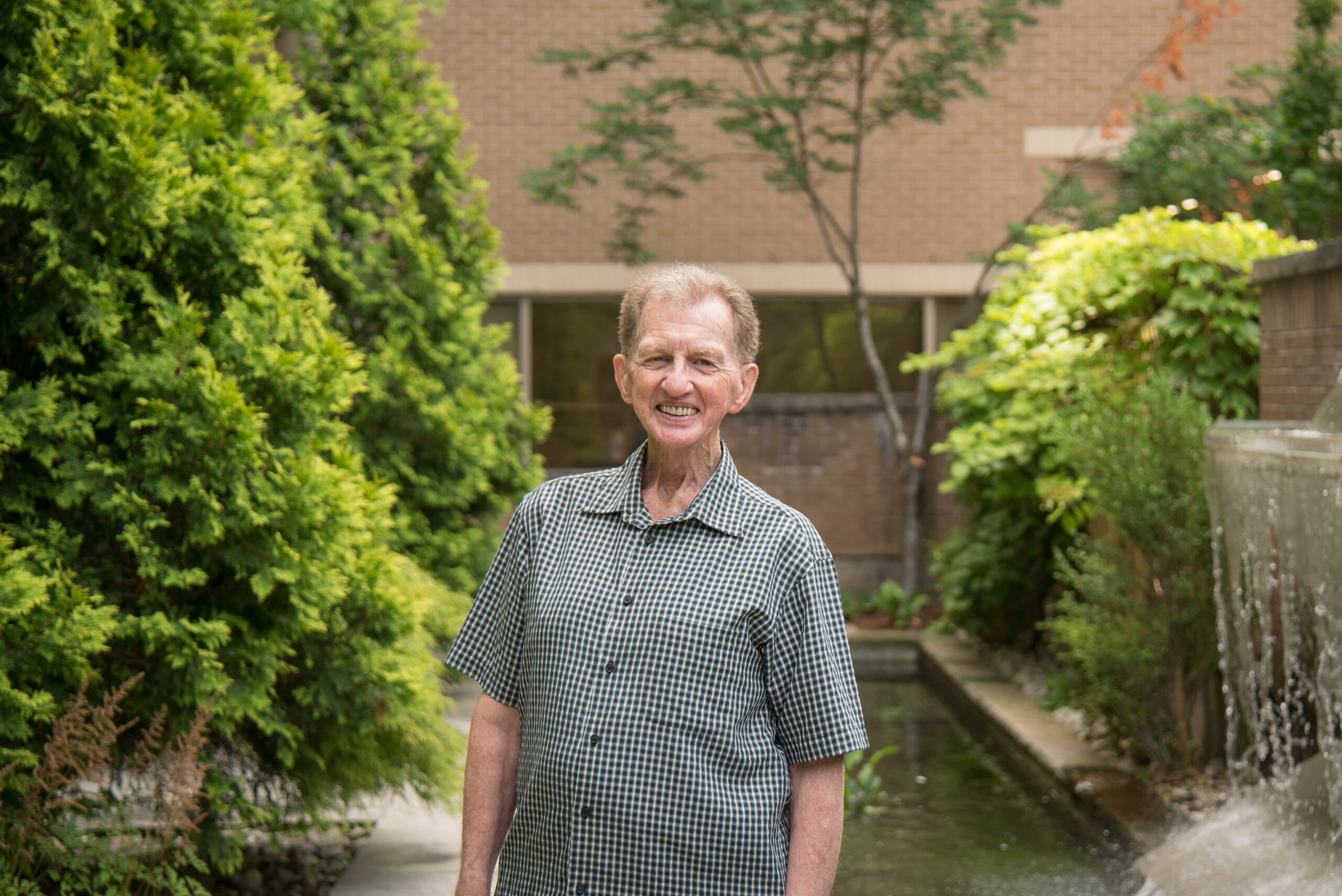
“The groundwork was laid by several people in the late ‘50s and early ‘60s,” says retired cardiologist Dr. Bill Kostuk. “When we started in 1972, we were unaware of the many major developments that would occur over the next 30 to 40 years. It was truly an amazing and wonderful time.”
Over the course of the next 50 years, UH’s Cardiac Care program – which includes both cardiology and cardiovascular surgery – would become one of the premier programs in Canada and build a reputation around the world.
Within the initial decade of operation, it would see its first heart transplant, conduct the world’s first operation to correct the life-threatening heart condition of right ventricle dysplasia, and announce plans to partner in what would become the John P. Robarts Research Institute that was created to focus on heart and brain research.
Dr. Kostuk was part of the team that did the first heart transplant at UH in 1981. It was also the first time in Canada the experimental anti-rejection drug, cyclosporine, was used. The late Dr. Neil McKenzie, who led the transplant surgery, recognized that rejection and infection are the main complications of a heart transplant, and for that, cyclosporine was a game changer. The first patient lived for 12 years afterward, and the second for 31 years.
Getting access to the cyclosporine was a coup for Dr. Cal Stiller who ultimately established the Canadian Centre for Transplantation in London in 1981 and the Walter J. Blackburn Multi-Organ Transplant Unit which opened in 1987. He arranged for UH to be a testing site for the drug that was discovered in Switzerland.
For Dr. McKenzie, who first joined LHSC as a senior resident in 1974, he found a home for his illustrious nearly 50-year career, where he also performed Canada’s first heart-lung transplantation, earning recognition as Canada’s foremost heart transplant surgeon.
Collaboration central to advancement
One highlight of working at UH was the collaboration within the Cardiac Care program between nurses and doctors, and between programs, such as with Dr. Charles Drake, a world-renown neurosurgeon who developed a technique to repair brain aneurysms that revolutionized their treatment. He was frequently known to come into the operating rooms to ask what the cardiac team was doing and to make observations as to what could be expected in terms of results. The two teams would sometimes operate together.
Cathy McGarrell, a retired nurse, started on the 6th floor at UH, then home to the Cardiac Care program, in 1973 and retired from full-time duties in 2007. Two highlights of her career were the addition of nurse practitioners to the unit and seeing the progress of going from bypass surgery to less invasive procedures such as angioplasty and stents to avoid open heart surgery.
“There were some pretty amazing things accomplished,” she says.
She also points out that there was great collaboration between nurses and doctors.
“I just have such great respect for what you saw with the surgeons and the nurses at that point in time,” she says. “There was a huge amount of respect between the two disciplines.”
Pioneers in their fields
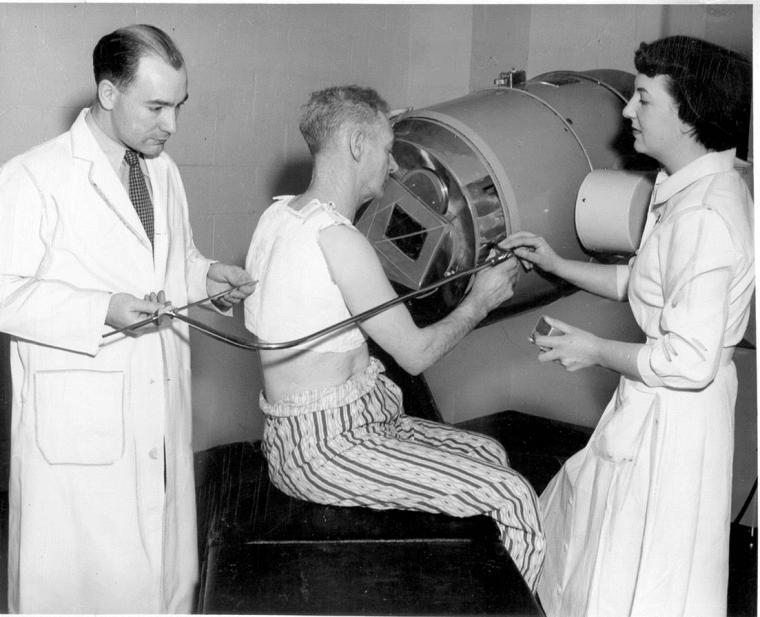
Dr. Ramsay Gunton was another pioneering cardiologist at UH. He was one of the first in Canada to develop the cardiac catheterization technique and was also a key member of the team that planned and developed London’s University Hospital and the John P. Robarts Research Institute. He was 92 when he died in 2015 after a short illness.
Another leading Canadian UH cardiologist is Dr. Derek Boughner. His work on echocardiography has involved the initial descriptions of its clinical applications and the early development of cardiac Doppler ultrasound. He was also involved in the development of the techniques and applicability of three-dimensional echocardiography.
Dr. George J. Klein, a world-renown electrophysiologist, or arrhythmia specialist, focused his research on cardiac arrhythmia and started the electrophysiology program at UH in 1980. Over the years, he and his colleagues have led the way in Canada for the management of patients with heart rhythm disorders.
And working alongside Drs. McKenzie and Kostuk in that first transplant using anti-rejection drugs, was cardiovascular surgeon, Dr. Raymond Heimbecker. Prior to joining UH, he performed the world’s first complete heart valve transplant in 1962. He was named an Officer of the Order of Canada in 1997 for his work. He passed away in 2014 at the age of 91.
Leaning into the future
As technology evolved over the years, LHSC came to play a pivotal role in robot-assisted surgery. In 1999, Dr. Doug Boyd headed a cardiac team, including Dr. Reiza Rayman, performing the world’s first robotic-assisted coronary artery bypass operation. This work led to the development of the specialty of robotic cardiac surgery and many world firsts at LHSC. Dr. Bob Kiaii continued developing new techniques and studies in robotic cardiac surgery, and ultimately LHSC became the exclusive training centre for the da Vinci robotic system in Canada.
Innovation and discovery have been a priority at UH with cardiac surgeons and cardiologists working together to develop new hybrid procedures that combine the best techniques with less-invasive approaches to enable faster patient recovery and improved quality of life.
Innovations have resulted in patients receiving leading edge care in transcatheter valve interventions, hybrid aortic operations, minimally invasive endoscopic valve repair, ventricular assist devices, and mechanical circulatory support, to name a few.
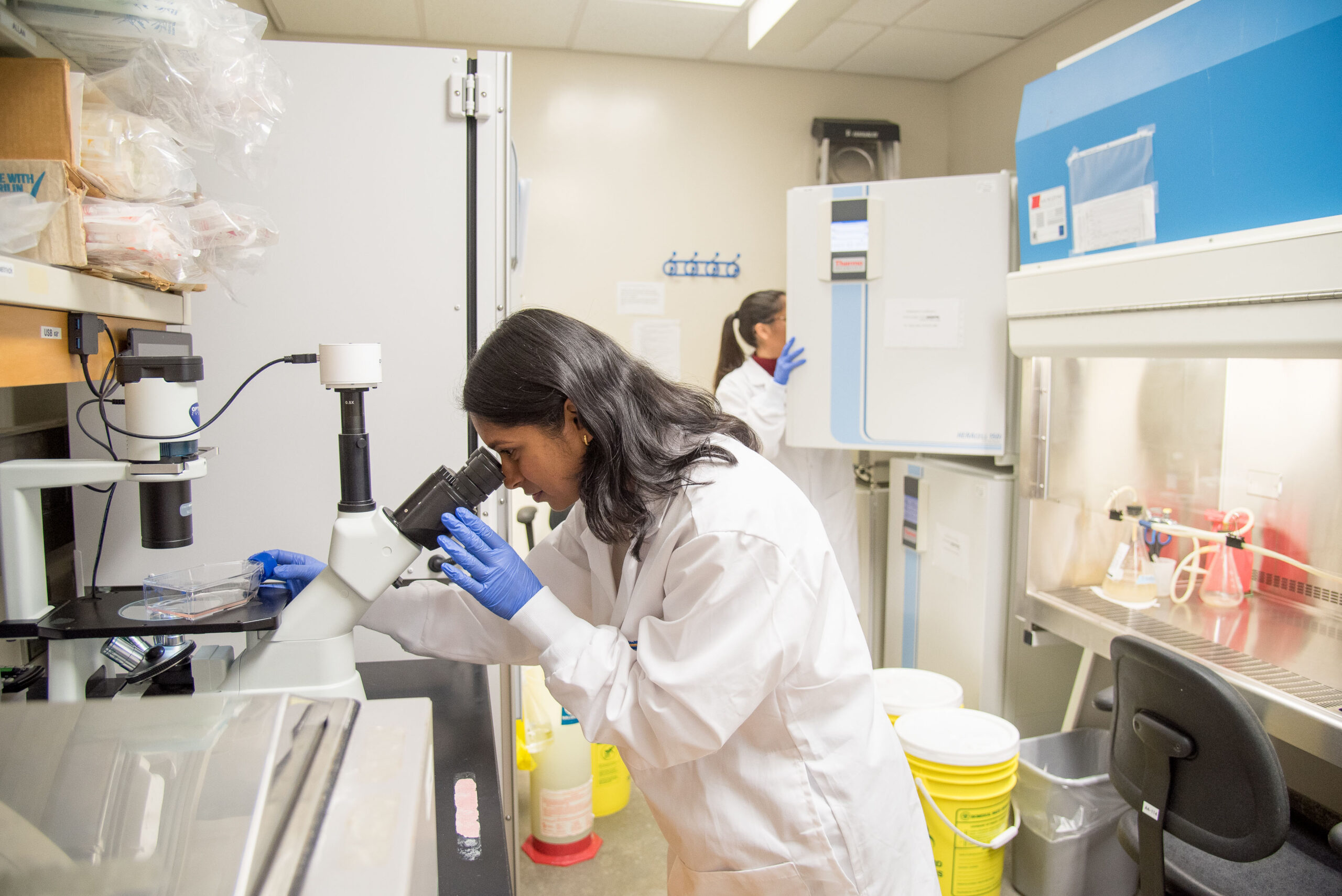
In addition, cardiac research programs through London Health Sciences Centre Research Institute (LHSCRI) have grown significantly and are attracting important grant support from some of the largest funding agencies. These research programs continue doing groundbreaking research that is being published in the most prominent medical journals.
Progression after progression
When Dr. Kostuk first walked into the new hospital building five decades ago, he couldn’t envision what the future would bring in the advancement of cardiac care and treatment or the role UH would play.
“It really has been a progression after progression. One thing led to another thing that led to better patient care in terms of diagnosing what the problem is and then being able to manage the problem for the patient,” he reflects.
“The developments over the last 50 years have really been phenomenal.”

LHSC is celebrating 150 years of care, innovation, and community impact by sharing 150 moments from our history. Join us in marking this milestone by sharing your own LHSC story.